Traumatic Brachial Plexus Injury
- Symptoms can mimic those of a spinal cord injury
- Essential to differentiate from spinal cord injury early
- Assume it is a spinal cord injury until proven otherwise
- Minor to moderate brachial plexus injuries are commonly referred to as “stingers” or “burners” which are transient, unilateral neuropraxias commonly seen in sporting injuries
- These will resolve without intervention and should be differentiated from more severe and permanent brachial plexus injuries
- Neurologic exam is critical to assess and document as the exam may change with time
- Common root injury patterns have classic resting arm positions (see below) which may help clue providers into specific roots that are injured
- Mechanism (often high energy)
- Often forced arm abduction i.e. grabbing a tree limb while falling
- “Stingers” are common sports injuries (often seen in football) and are unilateral and transient in nature (often paresthesias in deltoid and/or biceps)
- Timing of injury
- Other locations of injury or pain
- Numbness and tingling
- Variable distribution depending on the extent of injury (see physical exam)
- Associated injuries:
- Common: rib fractures, pneumothorax, clavicle fracture, closed head injuries, scapulothoracic dissociation
- Horner's syndrome (ptosis, miosis, anhidrosis)
- Anticoagulation? Last dose?
- Last time the patient ate (NPO)
- Hand dominance
- Profession
- Airway, breathing, circulation must be evaluated and stabilized with standard trauma evaluation guidelines
- Commonly occurs in high energy/level trauma setting
- Quick assessment of hemodynamic stability (heart rate, hypotension, etc.)
- Vascular injury can occur with traction injuries or direct trauma
- Assess the skin for lacerations, bruising, ecchymosis
- Tenderness to palpation
- Palpate the remainder of the upper extremity to assess for other injuries
- Palpate cervical spine for tenderness or step off
- Thorough secondary exam to assess for concomitant injuries
- Preganglionic injuries
- Horner's syndrome
- Ptosis, miosis, anhidrosis
- Winged Scapula
- Long thoracic nerve palsy
- Elevated hemidiaphragm
- Phrenic nerve palsy
- Postganglionic lesion
- Involves peripheral nervous system (see below)
- Careful exam to determine the extent of the injury and specific roots involved
- Do not have to localize roots acutely
- Document deficits in motion that you notice (for trending over time)
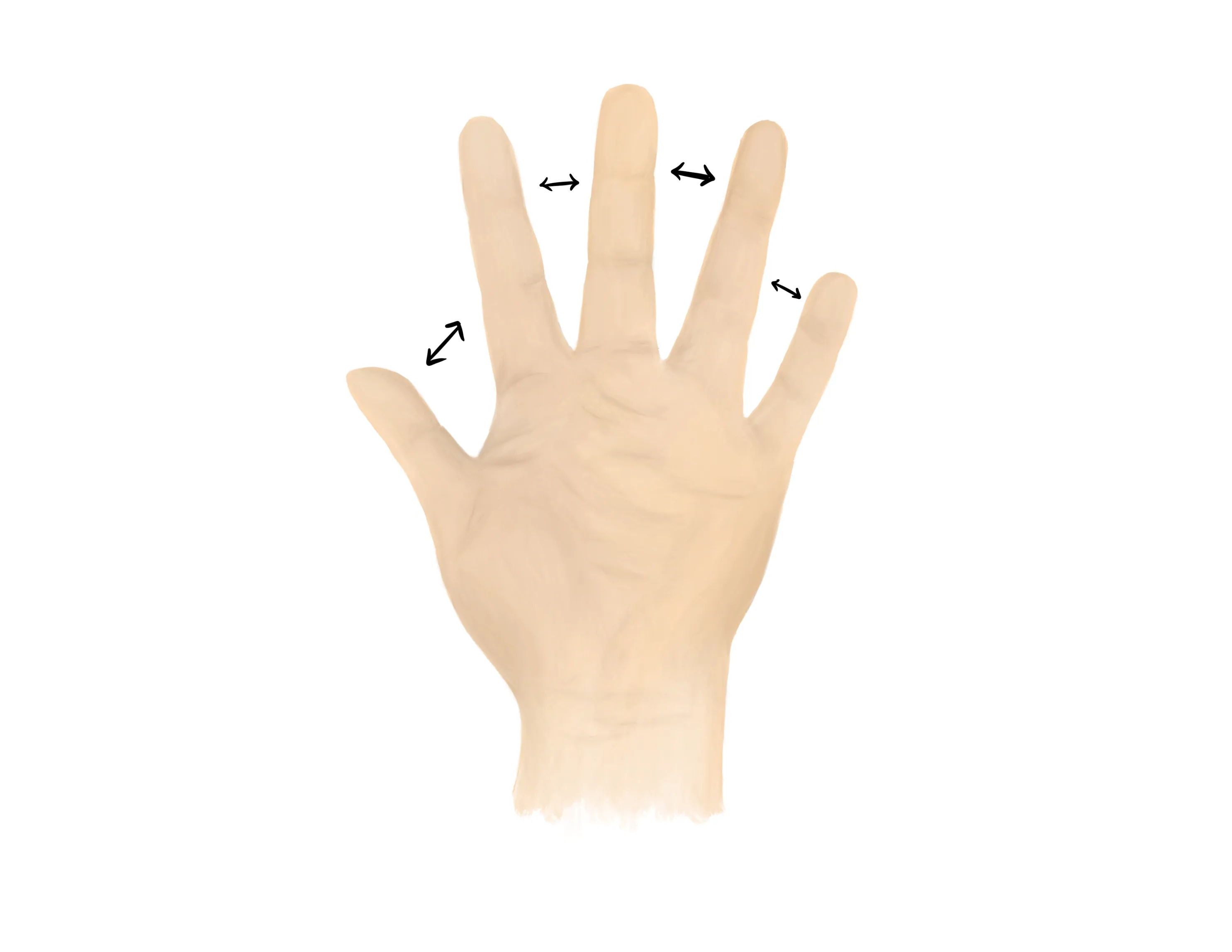
- Common Root Injury Patterns
- Complete involvement (C5-T1) - most common
- Worse prognosis
- Flaccid arm
- Involves motor and sensory
- C5-C6 upper trunk injuries
- Adducted, internally rotated at shoulder, pronated and extended at elbow

- Axillary nerve deficient (weak deltoid and teres minor)
- Musculocutaneous deficient (weak bicep)
- Suprascapular nerve deficient (weak supraspinatus and infraspinatus)
- C8-T1 lower trunk injuries

Motor Exam (common peripheral nerve exam) :
- Median Nerve/ Anterior interosseous nerve (AIN)
- Opposition of the thumb
- Opponens innervated by the median nerve - helpful to assess if concern for acute carpal tunnel syndrome
- Flexion of wrist, fingers, thumb
- “A-OK sign” = AIN
- Tests flexion of thumb IP joint (FPL) and flexion of index DIP joint (FDP)
- Radial nerve/ Posterior interosseous nerve (PIN)
-

- Extension of wrist, fingers, thumb
- Radial nerve palsy is common seen in humeral shaft fractures especially midshaft and distal third
- “Thumbs up” = PIN
- Tests extension of thumb IP and MCP joints (EPL))
- Palm on flat surface and lifting/extending thumb off the surface is also a good test for PIN (tests extension of thumb MCP joint (EPL))
- Ulnar nerve
- Radial artery, Ulnar artery
- If having difficulty with palpation of radial artery, find a US doppler
- Vascular injury can occur with traction injuries or direct trauma
- Capillary refill to digits
- Assess active motor function of the joints in the affected extremity
- May have motor deficits and be unable to move certain muscle groups
- PA/Lateral Chest
- Look for rib trauma and paralyzed diaphragm
- Cervical spine radiographs AP/L/Oblique/Odontoid view
- Transverse process fractures can indicate root avulsion
- Shoulder radiographs AP/L/Scapular Y/Axillary lateral vs. Velpeau
- Axillary lateral vs. Velpeau of shoulder
- Important to rule out concomitant shoulder dislocation which may not always be apparent on AP
- Consider Grashey view if concerned for intraarticular extension
- AP of the glenoid - possible to see fracture line exit into the glenoid
- Patient rotated 35-45 degrees and his or her back (scapular body) up against the imaging detector.
- CT myelography - Not acutely ordered
- Gold standard for nerve root injury definition
- Perform 3-4 weeks after injury
- MRI - Leave to discretion of orthopaedics to order
- Useful for imaging injuries distal to nerve roots and can visualize much of the plexus
Medical Decision Making
Traumatic Brachial Plexus Injury due to :
- Sharp penetrating trauma (excluding GSW)
- Iatrogenic injuries
- Open injuries
- Progressive neurologic decline
- Expanding hematoma or vascular injury
*** is a *** y/o ***R/L hand-dominant ***M/F presenting with pain to the ***R/L shoulder which occurred while ***mechanism, found to have a scapular fracture. The patient was neurovascularly intact and had no poke holes or punctate wounds. There was tenderness to palpation about the shoulder girdle and tenderness to palpation ***other locations. Imaging revealed ***. On ***velpeau/axillary lateral the glenohumeral joint was concentrically aligned. The patient was immobilized with a sling and will follow up with orthopedic surgery in a week.
Traumatic Brachial Plexus Injury due to/with:
- Closed injuries
- Traction injuries
- Signs of neurologic recovery
- GSW without vascular injury
*** year-old R/L***-hand dominant M/F*** with a history of *** presenting with R/L*** upper extremity injury following mechanism*** . There is *** motor deficit, and *** sensory deficit. There is/is not associated ***ptosis/ miosis/ anhidrosis. Associated injuries include ***. On examination the patient’s neurologic exam shows deficient ***C5/C6/C7/C8/T1. Vascular assessment shows a ***perfused hand with ***intact/deficient radial and ulnar pulse. Radiographs of the *** show ***. The injury is closed. Given the history, exam and imaging findings, a traumatic ***pre/post ganglionic brachial plexus injury is suspected on the ***R/L extremity involving *** nerve roots. Plan for immobilization in sling for comfort and close outpatient follow up with hand surgery in one week.
If Traumatic Brachial Plexus Injury due to :
- Sharp penetrating trauma (excluding GSW)
- Iatrogenic injuries
- Open injuries
- Progressive neurologic decline
- Expanding hematoma or vascular injury
- Consult orthopaedic surgery
- NPO, preop labs (type and screen, INR, aPTT, CBC, BMP)
- If concern for associated vascular injury- Consult vascular surgery immediately
- WB status: WBAT injured upper extremity, sling for comfort
- Diet: Regular
- Analgesia: short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 25 pills
- Immobilization
- Sling immobilization
- Disposition: Home with follow up in hand surgery clinic in 1 week
| Common ICD-10 Codes | Brief Description |
|---|---|
| S14.3 | Injury of brachial plexus |