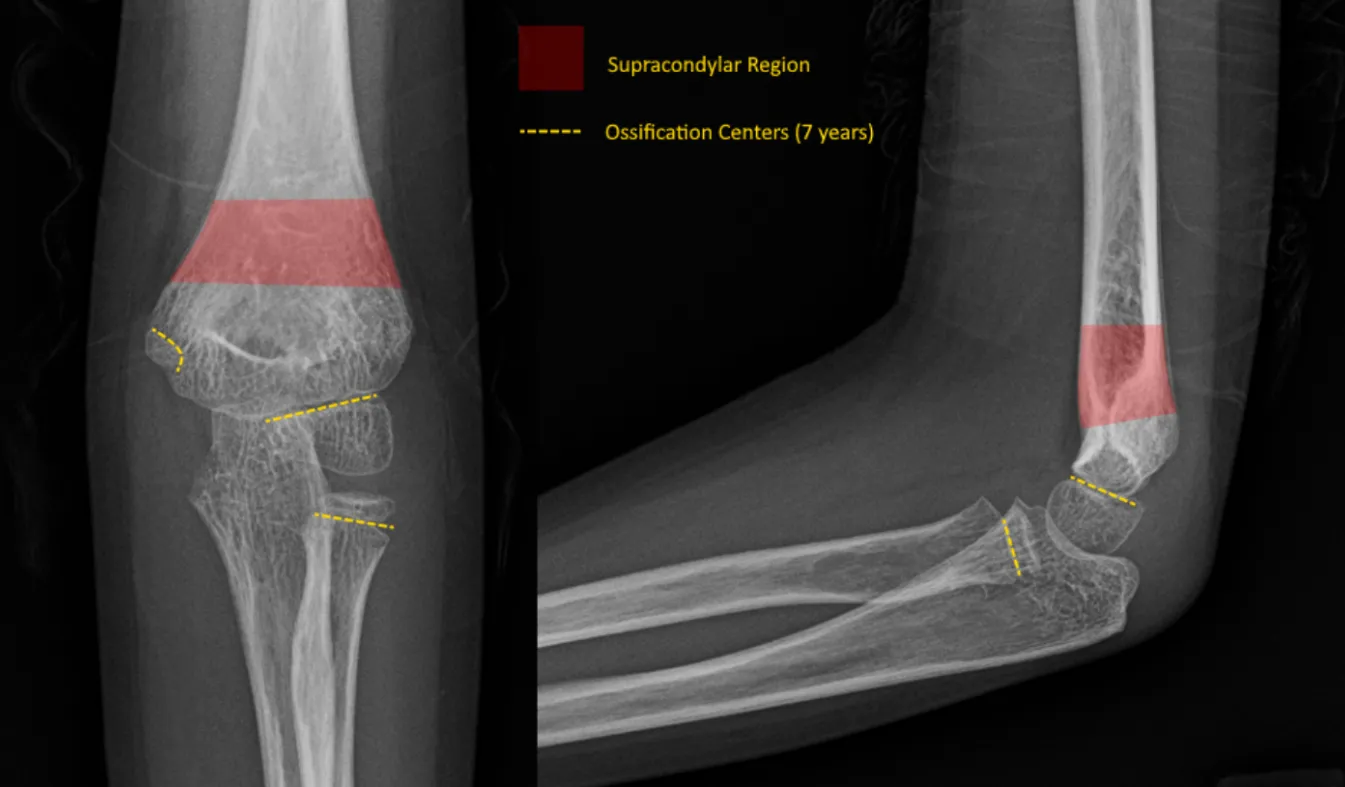
Pediatric Supracondylar Humerus Fracture
- Most common fracture in children
- Commonly presents in the younger children (5-9 years) with fall onto an outstretched hand (classic mechanism is fall of the monkey bars)
- Closed, minimally displaced fractures without neurovascular injury can be immobilized in a long arm splint and referred to orthopaedics within a week
- Open fractures, fractures associated with neurovascular injuries, and significantly displaced fractures require an orthopaedic consultation
- See Gartland Classification below
- A posterior “fat pad” sign is sometimes the only radiographic evidence of a fracture
- This radiographic feature is not specific to any single fracture but is often the only identifiable radiographic feature in occult fractures at the elbow
- If seen, place the arm in a long arm splint with orthopaedic follow up
- Mechanism
- Extension type: fall onto an outstretched hand with the elbow extended
- Flexion type: direct trauma or fall onto an outstretched hand with the elbow flexed
- Timing of injury
- Other locations of pain
- Numbness/tingling
- Can direct your attention to neurovascular deficits that are common with these fractures
- Be wary of compartment syndrome
- History of other broken bones?
- Vitamin D/Calcium deficiency
- Non-accidental trauma (abuse)
- Hand dominance (right versus left dominant handed)
- Time the patient last ate/drank (NPO status)
Vitals
- Remove any splint/wrapping to view the forearm
- Gross appearance of the forearm (deformity, soft tissue defect, pokeholes)
- Dimpling of antecubital skin - “Pucker sign” or “Brachialis sign”
- Fracture fragment gets entrapped in brachialis muscle and requires ‘milking’ maneuver to reduce through the brachialis
- Indicates a high energy trauma with significant displacement
- Higher risk for entrapment of median nerve and brachial artery,
- Higher risk of compartment syndrome
- Soft tissue defect/poke hole that probes to fracture = open fracture
- Small poke hole wounds near the fracture site with a slow, continuous ooze is indicative of an open fracture
- Do not miss this and confirm antibiotics were given
- Examine the forearm compartments (soft and compressible, firm but compressible, etc.)
- Palpate the hand, elbow, arm, and shoulder to identify concomitant injuries
- Ipsilateral forearm injuries with a supracondylar humerus fracture is termed a “floating elbow” and is associated with a higher risk of compartment syndrome
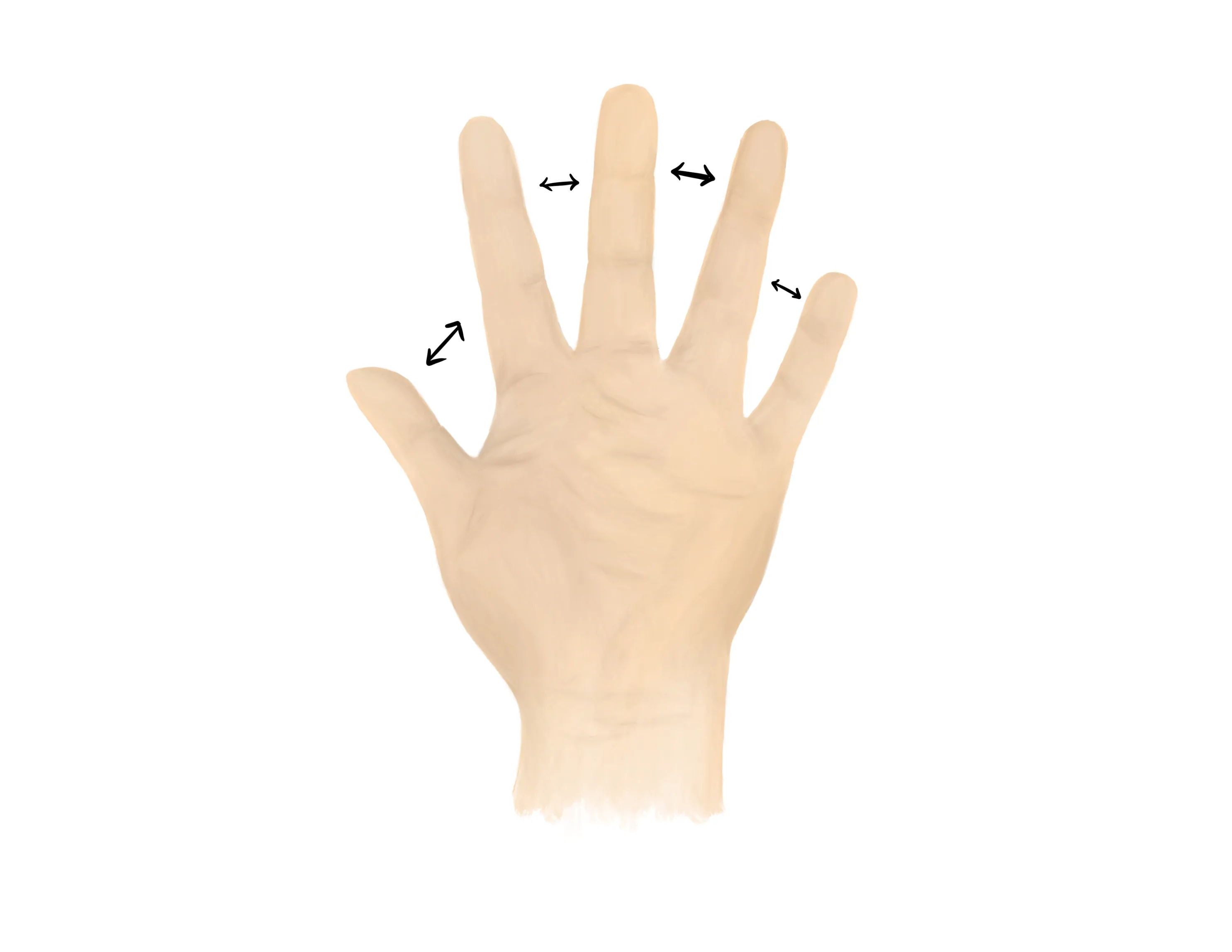
Motor Exam:
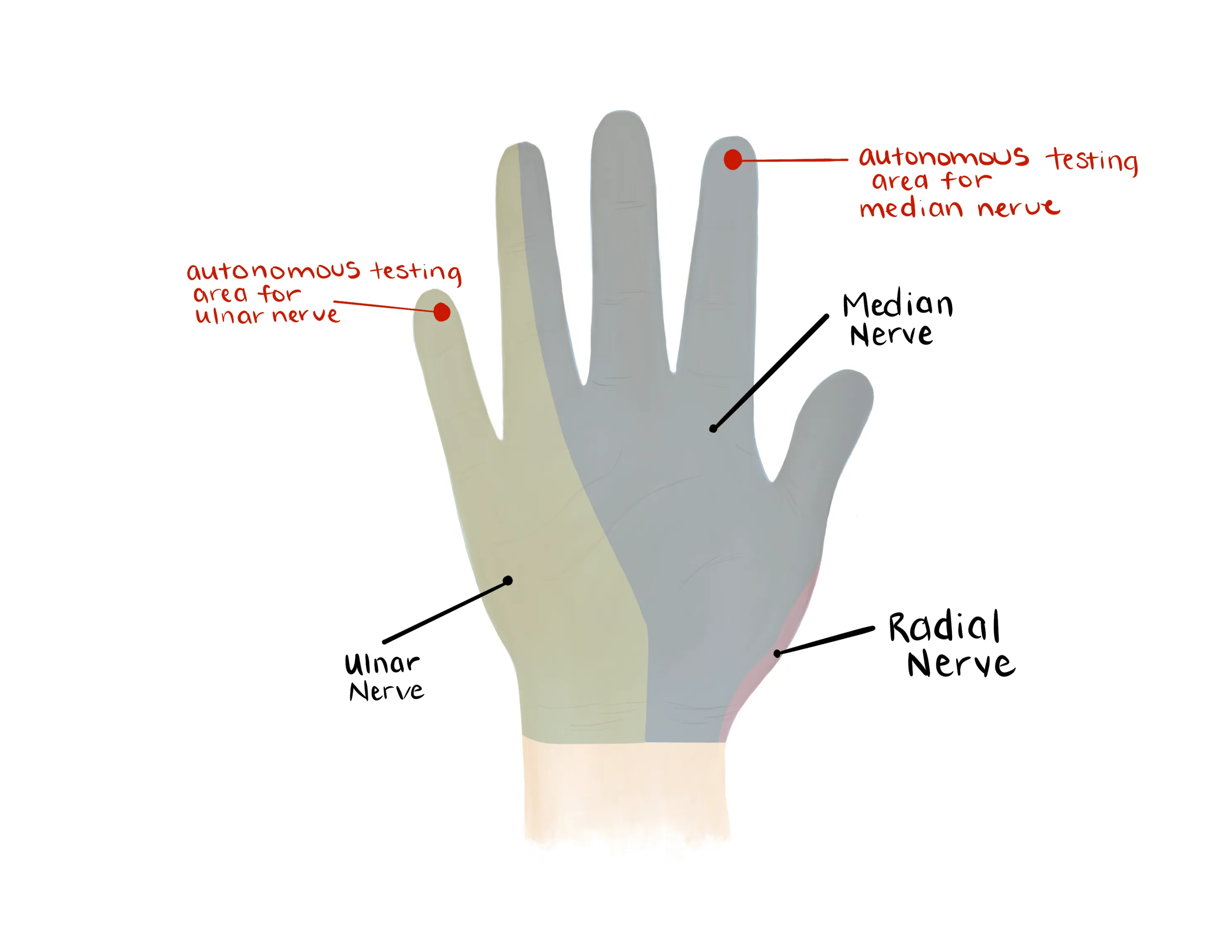
- Median Nerve/ Anterior interosseous nerve (AIN)
- AIN is the MOST COMMON neuropraxia with extension-type fractures (radial nerve is second most common)
- Flexion of wrist, fingers, thumb
- “A-OK sign” = AIN
- Test flexion of thumb IP joint (FPL) and flexion of index DIP joint (FDP)
- Radial nerve/ Posterior interosseous nerve (PIN)
-

- Extension of wrist, fingers, thumb
- “Thumbs up” = PIN
- Tests extension of thumb IP and MCP joints (EPL)
- Palm on flat surface and lifting/extending thumb off the surface is also a good test for PIN (tests extension of thumb MCP joint (EPL))
- Ulnar nerve
- Median, Radial, Ulnar nerve distributions
- Radial artery, Ulnar artery
- If having difficulty with palpation radial artery, find a doppler
- If pulseless, assess capillary refill (orthopaedics will ask immediately)
- Cool/white vs. warm/pink
- Consult orthopaedics immediately
- Capillary refill to digits
- AP/Lateral/Oblique elbow; AP/Lateral wrist
- To minimize the radiation dose, an AP and lateral of the elbow and forearm may be obtained in the same radiographs in the small/young patient
- A optimal AP and lateral of the elbow are required to determine the appropriate management
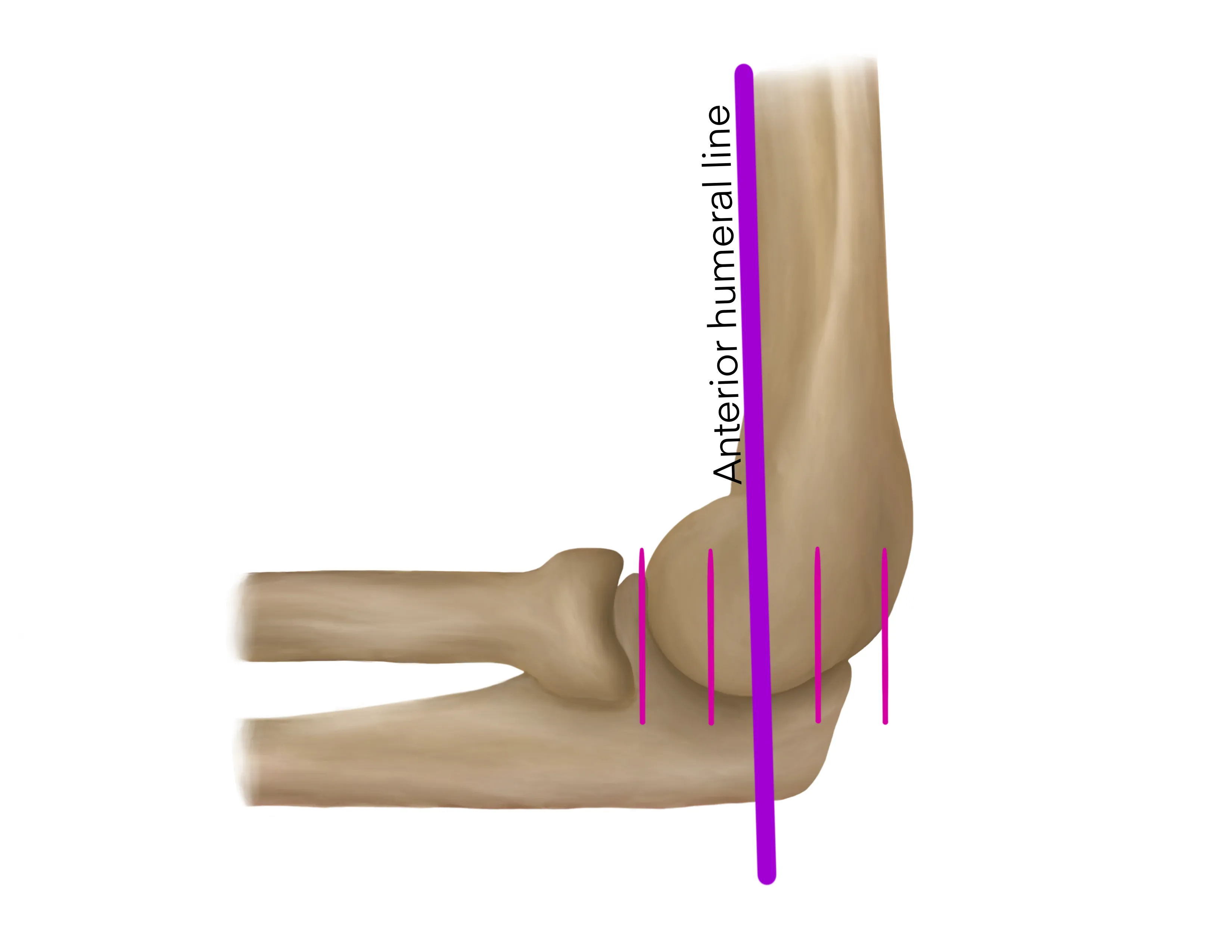
- Characterize the fracture - Prognostic and Disposition Implications
- Critical to utilize the anterior humeral line which is drawn down the anterior surface of the humerus and normally should bisect the middle ⅓ of the capitellum
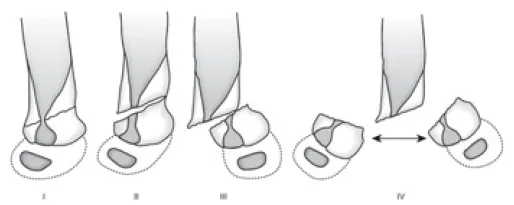
- Gartland Classification
- Types I-IV are extension type
- Type 1- Nondisplaced
- Anterior humeral line crosses too anteriorly relative to the capitellum
- Type 2- Displaced, sagittal plane only, anterior cortex disrupted, posterior cortex/periosteal hinge intact
- Type 3- Displaced in multiple planes, anterior and posterior cortex disrupted, however posterior periosteal hinge intact
- Type 4- Intraop diagnosis, displaced in multiple planes, periosteal hinge not intact
- * The only way to determine a type III from IV injury is intraoperatively
- Flexion type injury
-
Medical Decision Making
Closed Nondisplaced Supracondylar Fracture (Type 1):
*** is a *** y/o ***M/F with a history of *** presenting with an injury to the ***R/L elbow that occured while ***mechanism, found to have nondisplaced supracondylar fracture. The patient was neurovascularly intact with no poke holes, punctate wounds, or threatened skin. There was no pain with passive stretching of the fingers. Radiographs revealed a type 1 supracondylar fracture. The patient was placed in a long arm splint and will follow up with orthopaedics in 1 week.
Closed Displaced Supracondylar Fracture (Type 2/3) :
*** is a *** y/o ***M/F with a history of *** presenting with an injury to the ***R/L elbow that occured while ***mechanism, found to have displaced supracondylar fracture. The patient had a palpable radial pulse, normal capillary to the digits, and no poke holes, punctate wounds, or threatened skin at the elbow. The patient ***had/did not have a normal neurologic exam with an ***AIN/radial/ulnar nerve palsy. There was no pain with passive stretching of the fingers. Radiographs revealed a type 2/3*** supracondylar fracture. Orthopaedics was consulted and will provide further recommendations. The patient was made npo and last ate ***.
Open Supracondylar Fracture :
*** is a *** y/o ***M/F with a history of *** presenting with an injury to the ***R/L elbow that occured while ***mechanism, found to have an open supracondylar fracture. The patient had a palpable radial pulse, normal capillary to the digits. There was a laceration on the *** aspect of the elbow that probes to fracture. A dose of IV ***ancef/gentamicin was immediately administered. Gross contaminants were irrigated out of the wound at the bedside. The patient ***had/did not have a normal neurologic exam with an ***AIN/radial/ulnar nerve palsy. There was no pain with passive stretching of the fingers. Orthopaedics was consulted and will provide further recommendations. The patient was made npo and last ate ***.
Pulseless supracondylar fracture :
*** is a *** y/o ***M/F with a history of *** presenting with an injury to the ***R/L elbow that occured while ***mechanism, found to have a pulseless supracondylar fracture. The patient did not have a palpable radial pulse and no pulse was found on doppler ultrasound. The hand was/was not*** pink with normal/abnormal capillary refill. Orthopaedics was urgently consulted. There was no pain with passive stretching of the fingers. The patient was made npo and last ate ***.
Closed nondisplaced supracondylar fracture (Type 1) :
- WB status: Non-weight-bearing injured extremity
- Diet: regular
- Analgesia: short course of narcotic pain medication, tylenol (scheduled)
- Ex: weight-based Hycet, weight-based tylenol
- Immobilization
- Long arm splint
- Disposition: follow up with orthopaedic surgery within 1 week
- Regional/institutional/individual variations in practice for Type 2 supracondylar fractures
- Consult orthopaedic surgery
- WB status: Non-weight-bearing injured extremity
- Diet: per orthopaedic surgery (NPO until further recommendations are provided)
- Analgesia: short course of narcotic pain medication, tylenol (scheduled)
- Ex: weight-based Hycet, weight-based tylenol
- Immobilization
- Long arm splint
- Disposition: per orthopaedic surgery
- Type 3 supracondylar will be admitted for operative management
- Type 2 supracondylar may either be admitted for operative management, sent out with plan to manage via outpatient surgery, or managed nonoperatively in a cast at the discretion on the surgeon
- Consult orthopaedic surgery immediately
- NPO, preop labs (type and screen, INR, aPTT, CBC, BMP)
- Check tetanus status
- Ensure IV antibiotics were given (ancef, gentamicin)
- Gustillo-Anderson chart for antibiotic type and dose
- Institutional/individual variations in practice for pulseless supracondylar fractures
- Consult orthopaedic surgery immediately
- First question will be if the hand is warm/well perfused or cool/white
- Surgeon recommendations will be heavily predicated on this
- NPO, preop labs (type and screen, INR, aPTT, CBC, BMP)
Procedure Walkthroughs:
- Apply soft padding liberally around the upper arm at the level of the axilla, down the arm and forearm, and over the hand to the level of the distal palmar crease
- Measure plaster/Ortho-Glass on the posterior aspect of the upper arm, elbow, forearm, to the level of the posterior hand
- After wetting, lay the plaster/Ortho-Glass on the posterior aspect of the upper arm, elbow, forearm, to the level of the posterior hand
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with ace bandage or bias
Procedure Notes:
PROCEDURE NOTE ***R/L supracondylar humerus fracture
PRE-PROCEDURE DIAGNOSIS: fracture of the *** humeral shaft
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Application of long arm splint (shoulder to hand)
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient and parent/guardian agreed to proceed. A timeout was performed.
No attempts at reduction were made. A well-padded posterior slab, long arm splint was applied to the injured extremity in a semi flexed (< 90 degrees) position. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** humeral shaft
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Application of long arm splint (shoulder to hand)
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient and parent/guardian agreed to proceed. A timeout was performed.
No attempts at reduction were made. A well-padded posterior slab, long arm splint was applied to the injured extremity in a semi flexed (< 90 degrees) position. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
| Common ICD-10 Codes | Brief Description |
|---|---|
| S42.41 | Simple supracondylar fracture without intercondylar fracture of humerus |
| S42.42 | Comminuted supracondylar fracture without intercondylar fracture of humerus |
- Kropelnicki A, Ali AM, Popat R, Sarraf KM. Paediatric supracondylar humerus fractures. Br J Hosp Med (Lond). 2019;80(6):312-316. doi:10.12968/hmed.2019.80.6.312
- Mulpuri K, Wilkins K. The treatment of displaced supracondylar humerus fractures: evidence-based guideline. J Pediatr Orthop. 2012;32 Suppl 2:S143-S152. doi:10.1097/BPO.0b013e318255b17b
- Tintinalli, J. E., Stapczynski, J. S., Ma, O. J., Yealy, D. M., Meckler, G. D., & Cline, D. (2016). Injuries to Bones and Joints In Tintinalli's emergency medicine: A comprehensive study guide (Eighth edition.) (pp1863-1864). New York: McGraw-Hill Education.
- Davenport M. Procedures for orthopedic emergencies. In: Bond M, ed. Orthopedic Emergencies: Expert Management for the Emergency Physician. Cambridge: Cambridge University Press; October 31, 2013.