Scaphoid Fracture
- General
- Most common carpal bone fracture
- Commonly missed, often an occult fracture
- Retrograde blood supply
- At risk for nonunion and avascular necrosis
- 10% risk of nonunion for nondisplaced waist fractures treated nonoperatively
- 50% risk of nonunion for displaced waist fractures treated nonoperatively
- Immobilization & WB Status
- Thumb spica splint
- Non-weight-bearing injured arm
- Disposition
- Closed fracture: follow up with orthopedic surgery within 1 week
- Express the importance of follow up to the patient, given risk for avascular necrosis of this fracture pattern (frequently requires outpatient surgery)
- Open fracture (extremely rare): consult to orthoapedic surgery; admission
- Mechanism
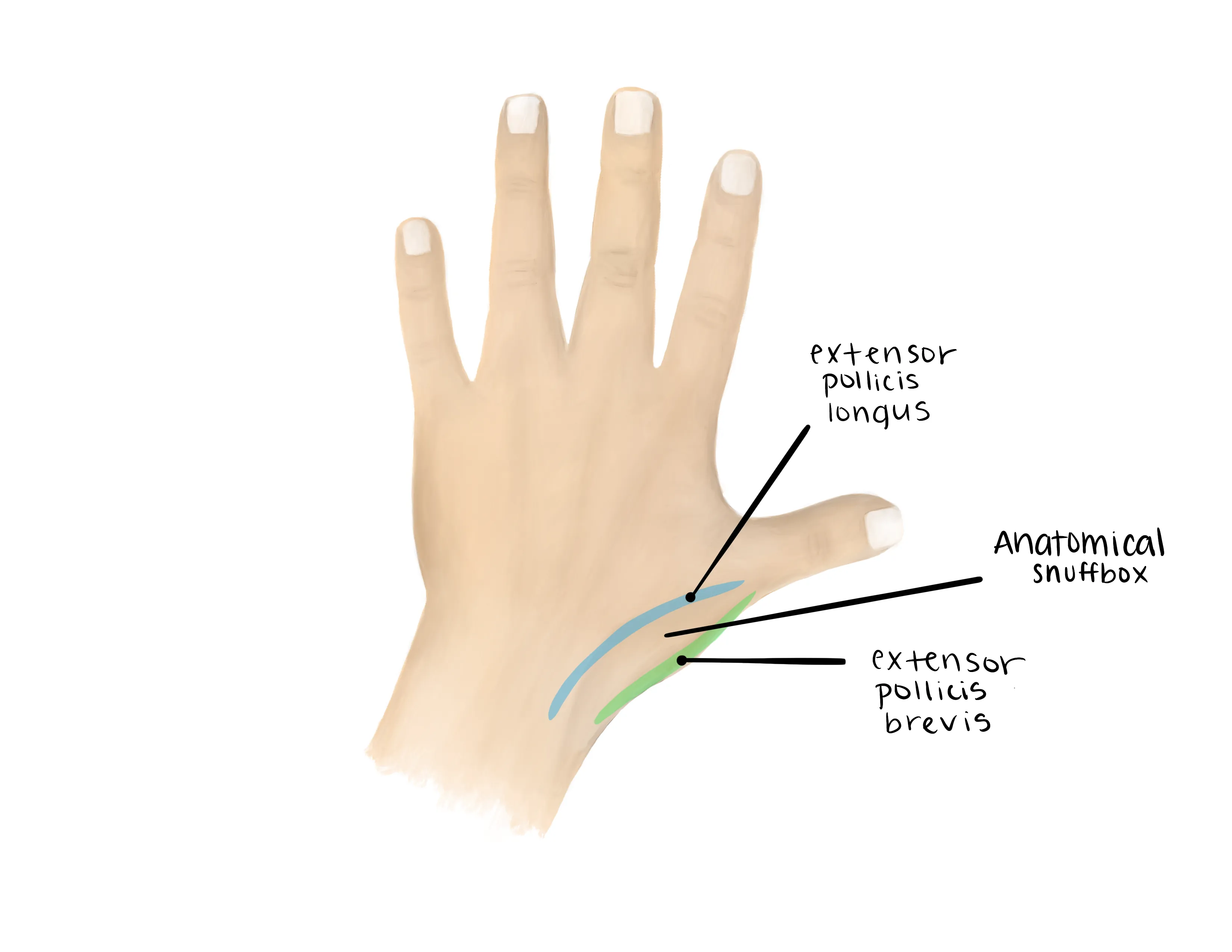
- Have a high index of suspicion for wrist pain & snuffbox tenderness
- Commonly: fall on outstretched arm, MVC, contact sports
- Timing of injury
- Missed injuries can lead to scaphoid nonunion and arthritis
- Other locations of pain
- Often occurs with other fractures of the distal radius and carpal bones
- Numbness/Tingling
- Hand dominance
- Profession
- Tobacco use
- Poor healing potential and higher risk of osteonecrosis
Vitals
Motor Exam:
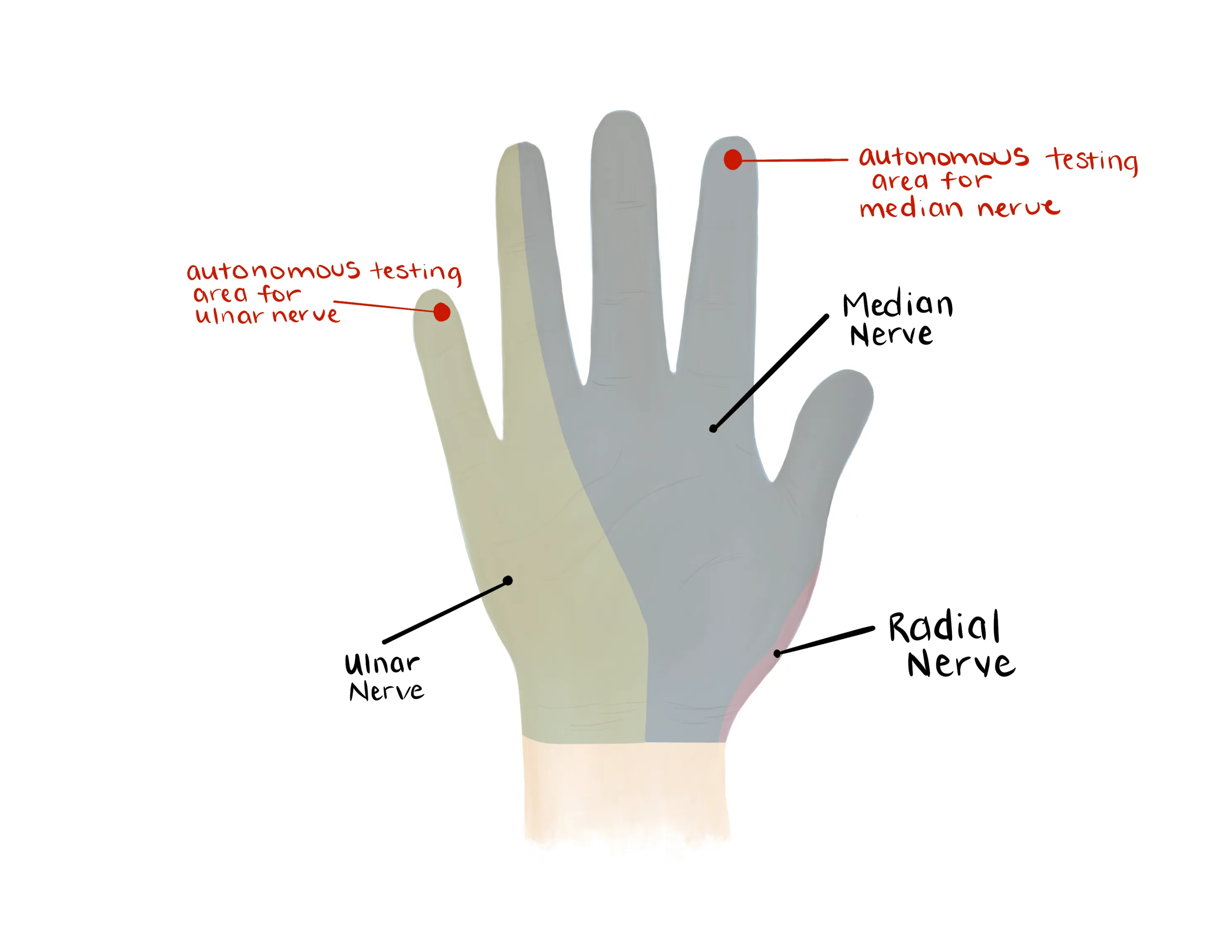
- Median Nerve/ Anterior interosseous nerve (AIN)
- Flexion of wrist, fingers, thumb
- “A-OK sign” = AIN
- Tests flexion of thumb IP joint (FPL) and flexion of index DIP joint (FDP)
- Radial nerve/ Posterior interosseous nerve (PIN)
-

- Extension of wrist, fingers, thumb
- “Thumbs up” = PIN
- Tests extension of thumb IP and MCP joints (EPL)
- Palm on flat surface and lifting/extending thumb off the surface is also a good test for PIN (tests extension of thumb MCP joint (EPL))
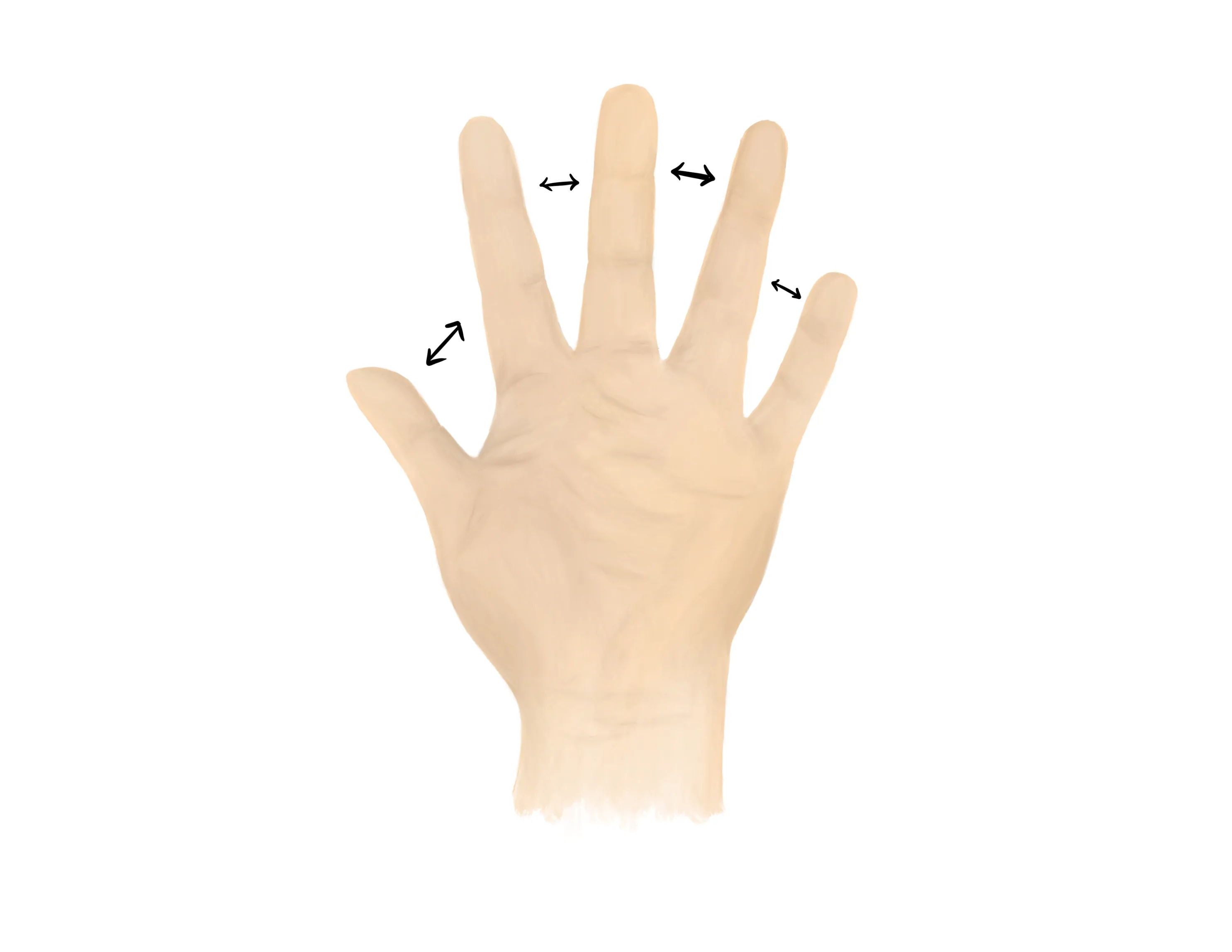
- Ulnar nerve
- Median, Radial, Ulnar nerve distributions
- Radial artery, Ulnar artery
- Capillary refill to digits
- Extension of digits and wrist
- Often pain limited at the wrist
- Flexion of the digits and wrist
- Often pain limited at the wrist
- Pain exacerbated with circumduction of the wrist
- Radiographs AP/lateral/oblique of involved wrist, hand, and forearm
- Up to 25% of scaphoid fractures are not visible on radiographs
- Treat the patient for occult fracture as these can be subtle injuries that are very difficult to see on initial imaging
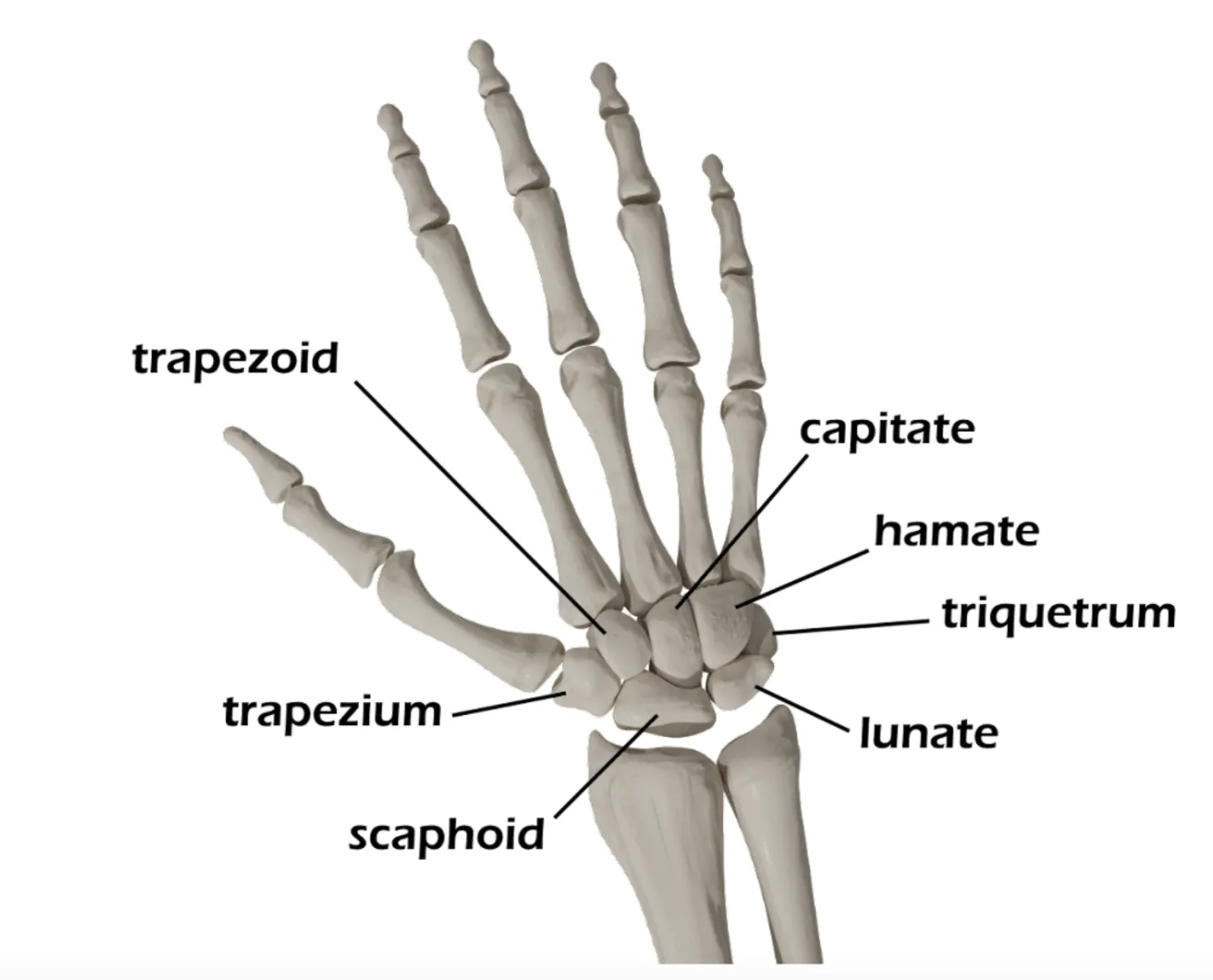
- Ensure there is not a concomitant perilunate dislocation or lunate dislocation
- Special views to consider
- Scaphoid view: -30 degrees of wrist extension, 20 degrees of ulnar deviation
- Clenched fist view: AP radiograph while grasping a pen or pencil
- CT scan
- Provides details of other carpal bone fractures
- Helpful in cases where clinical index of suspicion is high with equivocal X-rays
- MRI - rarely necessary in the ED
- Most sensitive for occult fractures
Medical Decision Making
Concern for a Scaphoid Fracture :
*** is a *** y/o ***-hand dominant ***M/F with hx of ***, who presents with an injury to the *** upper extremity and concern for a scaphoid fracture after mechanism***. On exam, the patient is neurovascularly intact. There is pain in the anatomic snuff box and pain with axial loading of the thumb. The injury is closed and isolated. Radiographs do not reveal an obvious fracture line. Given the clinical presentation consistent with an occult scaphoid fracture, the patient was placed in a thumb spica splint. The patient will follow up with orthopedic surgery within one week for repeat evaluation.
Radiographically Visible Closed Scaphoid Fracture :
*** is a *** y/o ***-hand dominant ***M/F with hx of ***, who presents with an injury to the *** upper extremity after mechanism***, found to have scaphoid fracture. On exam, the patient is neurovascularly intact. There is pain in the anatomic snuff box and pain with axial loading of the thumb. The injury is closed and isolated. Radiographs ***. The patient was placed in a thumb spica splint. The patient will follow up with orthopedic surgery within one week for repeat evaluation.
Open Scaphoid Fracture :
*** is a *** y/o ***-hand dominant ***M/F with hx of ***, who presents with an injury to the *** upper extremity after mechanism***, found to have an open scaphoid fracture. On exam, the patient is neurovascularly intact. There is a ***cm laceration on the *** aspect of the wrist which probes to fracture. A dose of ancef (***2/3g) was given immediately and gross contaminants were irrigated out of the wound at bedside. Radiographs revealed ***. Orthopaedics was consulted and the patient was made npo. The patient last ate at ***.
Open scaphoid fracture:
- Consult orthopedic surgery
- NPO
- Ensure IV cefazolin (2-3g) were given
- Assess tetanus status
- Gustillo-Anderson chart for antibiotic type and dose
- Depending on the size of the soft tissue defect may require gentamicin as well
- WB Status: Non-weight-bearing injured hand and wrist
- Diet: Regular
- Analgesia: short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 15 pills
- Immobilization
- Thumb spica splint
- Thumb in neutral position as if holding a can of soda
- Disposition: Home with follow up in orthopedic surgery clinic in 1 week
Procedure Walkthroughs:
- Thumb spica splint
- Position: as if holding a can of soda
- Apply soft padding liberally over the thumb, wrist, and distal forearm
- Split the plaster/orthoglass longitudinal with its length on one side
- After wetting, use the split end to cocoon the first ray with the hand in the position as if holding a can of soda
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with an elastic or nonelastic wrap based on personal or institutional preference
Procedure Notes:
PROCEDURE NOTE Closed treatment of carpal scaphoid (navicular) fracture; without manipulation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** scaphoid
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of carpal scaphoid (navicular) fracture; without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, stiffness, numbness, and tingling. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
A well-padded thumb spica splint was applied to the injured hand. Post splint radiographs showed unchanged alignment after the in-situ splinting. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** scaphoid
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of carpal scaphoid (navicular) fracture; without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, stiffness, numbness, and tingling. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
A well-padded thumb spica splint was applied to the injured hand. Post splint radiographs showed unchanged alignment after the in-situ splinting. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
| Common ICD-10 Codes | Brief Description |
|---|---|
| S62.0 | Fracture of navicular [scaphoid] bone of wrist |
| S62.01 | Fracture of distal pole of navicular [scaphoid] bone of wrist |
| S62.02 | Fracture of middle third of navicular [scaphoid] bone of wrist |
| S62.03 | Fracture of proximal third of navicular [scaphoid] bone of wrist |
- Tintinalli, J. E., Stapczynski, J. S., Ma, O. J., Yealy, D. M., Meckler, G. D., & Cline, D. (2016). Injuries to Bones and Joints In Tintinalli's emergency medicine: A comprehensive study guide (Eighth edition.) (pp1863-1864). New York: McGraw-Hill Education.
- Davenport M. Procedures for orthopedic emergencies. In: Bond M, ed. Orthopedic Emergencies: Expert Management for the Emergency Physician. Cambridge: Cambridge University Press; October 31, 2013.


.webp?&w=600&h=600&fit=clip)


