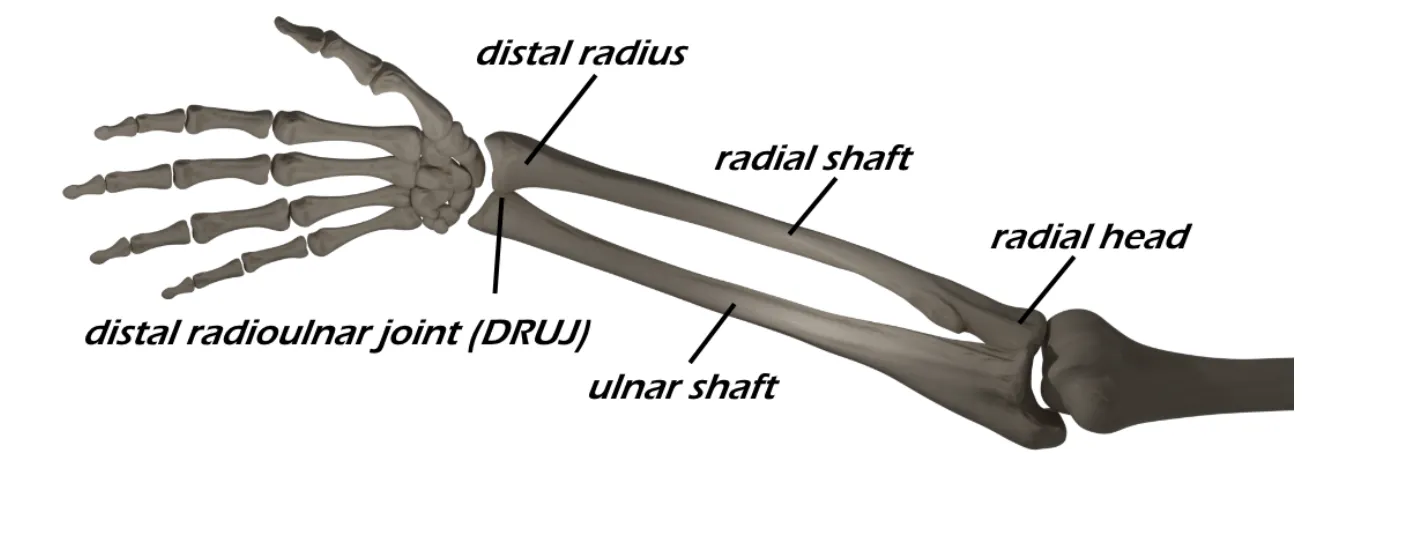
Radius and Ulnar Shaft Fractures
- Common patterns
- Two-bone (Both-bone) forearm fx: fractures of both the radial and ulnar shafts
- Nightstick fx: fracture of ulnar shaft without fracture or dislocation of the radius
- Monteggia fx: fracture of ulnar shaft with radial head dislocation
- Galeazzi fx: fracture of the radial shaft with disruption of the distal radioulnar joint
- Grossly displaced fractures should be reduced and splinted in the ED to prevent neurovascular injury and to relieve pain
- Mechanism
- Timing of injury
- Other location of pain
- Elbow - radial head dislocation
- Wrist - distal radioulnar joint disruption
- Numbness and tingling in ipsilateral UE
- Be wary of compartment syndrome
- Hand dominance (right vs. left hand dominant)
- Profession
- Anticoagulation
- Last dose?
- Last time the patient ate (NPO status)
Vitals
- Gross appearance of the forearm (deformity, soft tissue defect, pokeholes)
- Soft tissue defect/poke hole that probes to fracture = open fracture
- Small poke hole wounds near the fracture site with a slow, continuous ooze is indicative of an open fracture
- Do not miss this and confirm antibiotics were given
- Examine the forearm compartments (soft and compressible, firm but compressible, etc.)
- Pain with passive stretch of the fingers is concerning for compartment syndrome
- High risk fracture for compartment syndrome
- Palpate the hand, wrist, elbow, arm and shoulder to identify concomitant injuries
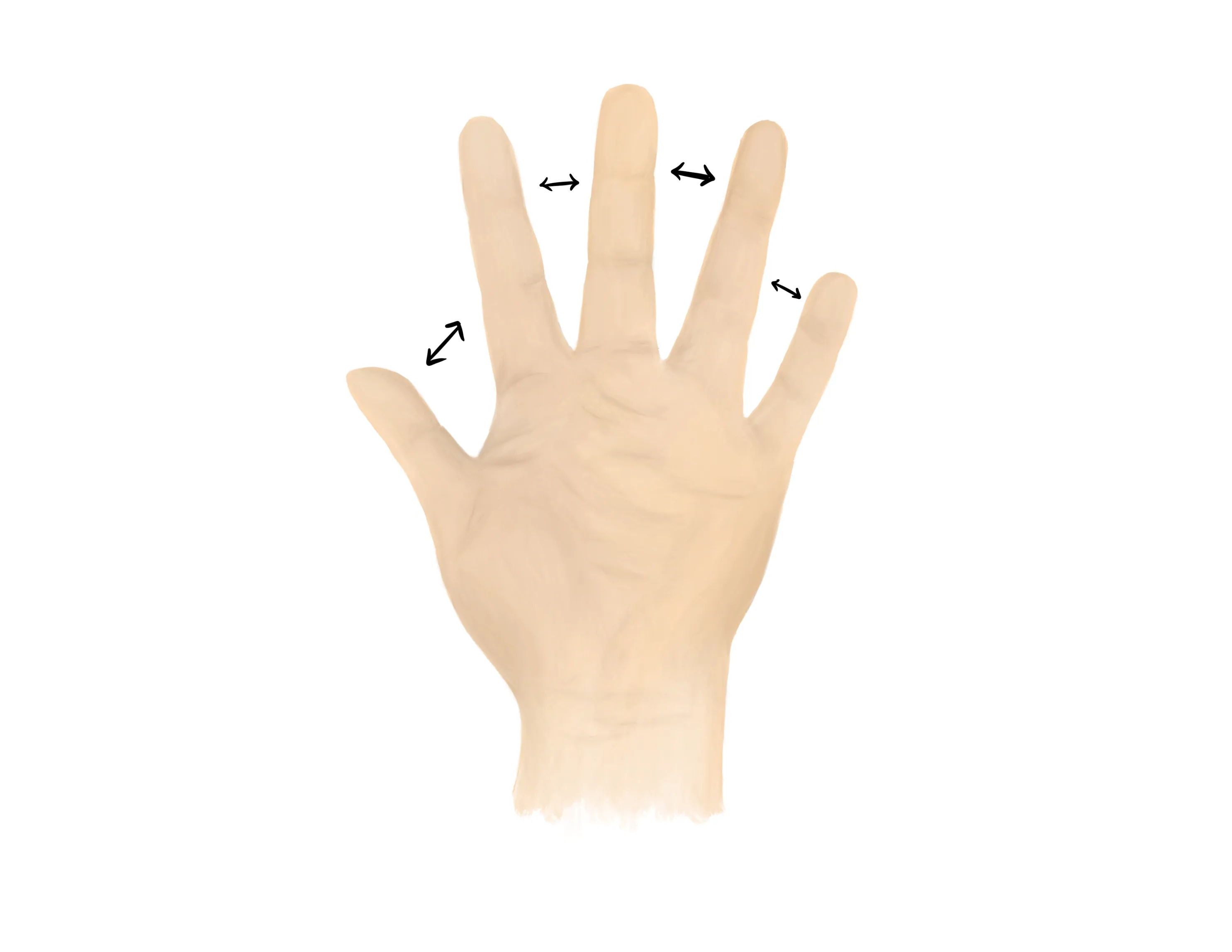
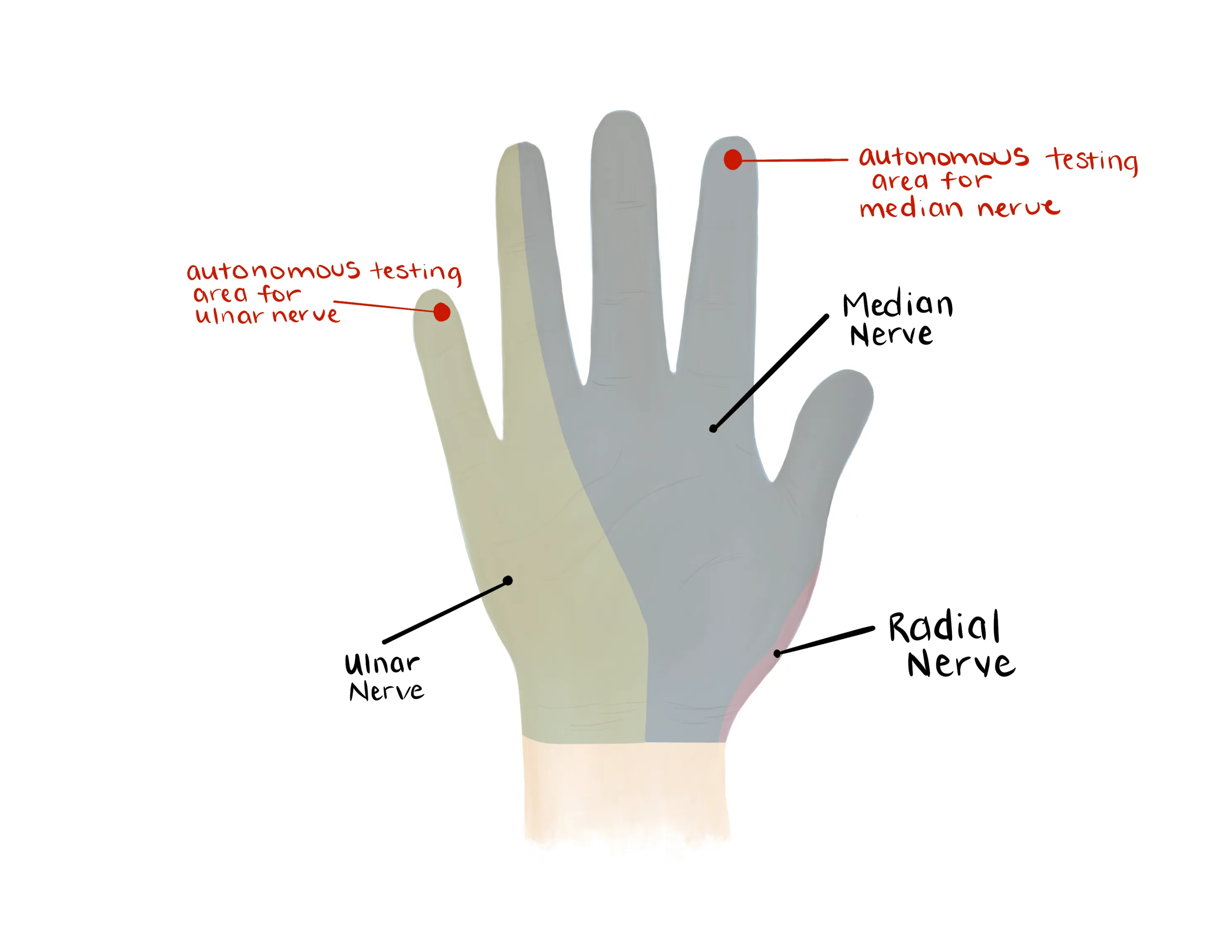
Motor Exam:
- Median Nerve/ Anterior interosseous nerve (AIN)
- Opposition of the thumb
- Opponens innervated by the median nerve - helpful to assess if concern for acute carpal tunnel syndrome
- Flexion of wrist, fingers, thumb
- “A-OK sign” = AIN
- Tests flexion of thumb IP joint (FPL) and flexion of index DIP joint (FDP)
- Radial nerve/ Posterior interosseous nerve (PIN)
-

- Extension of wrist, fingers, thumb
- “Thumbs up” = PIN
- Tests extension of thumb IP and MCP joints (EPL))
- Palm on flat surface and lifting/extending thumb off the surface is also a good test for PIN (tests extension of thumb MCP joint (EPL))
- Ulnar nerve
- Median, Radial, Ulnar nerve distributions
- Radial artery, Ulnar artery
- If having difficulty with palpation radial artery, find a doppler
- Capillary refill to digits
- ROM of the wrist and elbow likely limited secondary to pain
Medical Decision Making
Closed Radial & Ulnar Shaft Fractures (not c/f compartment syndrome):
*** is a *** y/o ***R/L hand-dominant individual with a history of *** presenting with an injury to the *** forearm which occurred while ***, found to have radial and ulnar shaft fractures. On exam, the patient is neurovascularly intact with no poke holes or punctate wounds. Compartments are full but compressible with no pain with passive stretch. There is tenderness to palpation and localized edema about the fracture site. Radiographs reveal ***. The injury was/was not *** reduced and the patient was immobilized with a sugar tong splint and will follow up with orthopedic surgery in one week.
Closed Radial & Ulnar Shaft Fractures (with c/f compartment syndrome):
*** is a *** y/o ***R/L hand-dominant individual with a history of *** presenting with an injury to the *** forearm which occurred while ***, found to have radial and ulnar shaft fractures. On exam, the patient is neurovascularly intact with no poke holes or punctate wounds. Compartments are full with rapidly worsening pain and exacerbation of pain with passive stretch. Radiographs reveal ***. Hand surgery was consulted urgently for evaluation for compartment syndrome. The patient was made npo and last ate at ***.
Open Radial & Ulnar Shaft Fractures:
*** is a *** y/o ***R/L hand-dominant individual with a history of *** presenting with an injury to the *** forearm which occurred while ***, found to have open ulnar and radial shaft fractures. On exam, the patient is neurovascularly intact with an open wound on the ***location on arm. The patient was immediately given a dose of IV ancef/gentamicin***. Radiographs reveal ***. Orthopaedics was consulted and the patient was kept NPO. The fracture was immobilized in a sugar tong splint. Orthopaedic surgery to admit the patient and assume care.
If open fracture:
- Consult orthopaedic surgery immediately
- NPO, preop labs (type and screen, INR, aPTT, CBC, BMP)
- Ensure IV antibiotics were given (ancef, gentamicin)
- Gustillo-Anderson chart for antibiotic type and dose
- Consult orthopaedic surgery immediately
- NPO, preop labs
- WB status: Nonweightbearing injured upper extremity
- Diet: Regular
- Analgesia: short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 25 pills
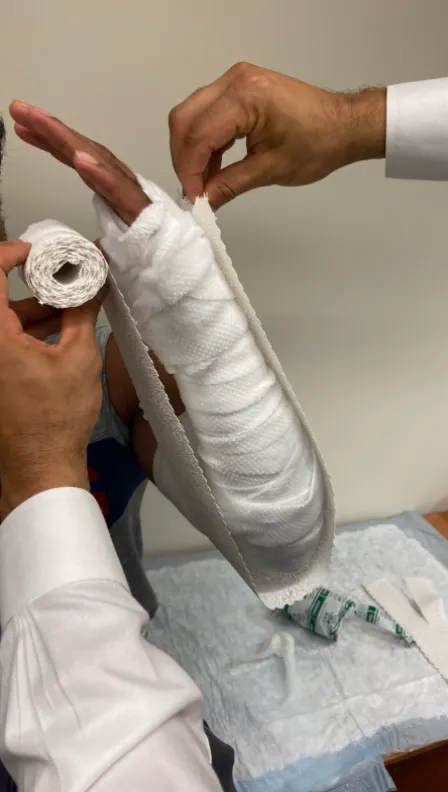
- Immobilization
- Sugar Tong Splint +/- reduction
- If grossly aligned, arm should be splinted without reduction
- If grossly malaligned, attempt closed reduction & splinting
- Reduction is rarely performed for these fractures as they usually will still require subsequent operative intervention
- As always, if you feel uncomfortable with the reduction, consult hand surgery
- Disposition: Home with follow up in orthopedic surgery clinic in 1 week
Materials for Splint
Procedure Walkthroughs:
- Apply soft padding liberally over elbow, forearm, and palm up to the level of the distal palmar crease
- Measure plaster/Ortho-Glass from the mid-palm over the volar surface of the forearm, around the elbow, and over the dorsal surface of the forearm to the same level distally
- After wetting, lay the plaster/Ortho-Glass from the mid-palm over the volar surface of the forearm, around the elbow, and over the dorsal surface of the forearm to the same level distally
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with ace bandage or bias
- Provide IV narcotics (ex. 1mg dilaudid) +/- anxiolytic (2mg midazolam)
- Assess grossly visible angulated deformity and apply traction and countertraction and a force opposing the apex of the deformity to correct it
- Apply soft padding liberally over elbow, forearm, and palm up to the level of the distal palmar crease
- Measure plaster/Ortho-Glass from the mid-palm over the volar surface of the forearm, around the elbow, and over the dorsal surface of the forearm to the same level distally
- After wetting lay the plaster/Ortho-Glass from the mid-palm over the volar surface of the forearm, around the elbow, and over the dorsal surface of the forearm to the same level distally
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with ace bandage or bias
- Mold the splint with an interosseous mold (squeezing the splint from volar and dorsal)
Procedure Notes:
PROCEDURE NOTE Closed treatment of radial and ulnar shaft fractures; without manipulation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** radial and ulnar shaft
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of radial and ulnar shaft fractures; without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempts at reduction were made. A well-padded sugar tong splint was applied to the injured extremity. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** radial and ulnar shaft
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of radial and ulnar shaft fractures; without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempts at reduction were made. A well-padded sugar tong splint was applied to the injured extremity. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE Closed treatment of radial and ulnar shaft fractures; with manipulation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** radial and ulnar shaft
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV ***narcotic
NAME OF PROCEDURE: Closed treatment of radial and ulnar shaft fractures; with manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
The gross angulation of the forearm was corrected with traction and countertraction and force opposing the apex of deformity. After the maneuver, the angulation was noted to be significantly improved from prior. A well-padded sugar tong splint was applied to the injured extremity with an interosseous mold. The patient's neurovascular status was consistent with baseline. Additional imaging was/was not*** obtained.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** radial and ulnar shaft
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV ***narcotic
NAME OF PROCEDURE: Closed treatment of radial and ulnar shaft fractures; with manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
The gross angulation of the forearm was corrected with traction and countertraction and force opposing the apex of deformity. After the maneuver, the angulation was noted to be significantly improved from prior. A well-padded sugar tong splint was applied to the injured extremity with an interosseous mold. The patient's neurovascular status was consistent with baseline. Additional imaging was/was not*** obtained.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
| Common ICD-10 Codes | Brief Description |
|---|---|
| M84.339 | Stress fracture, unspecified ulna and radius |
| M84.439 | Pathological fracture, unspecified ulna and radius |
| S52.2 | Fracture of shaft of ulna |
| S52.3 | Fracture of shaft of radius |
| S52.**1 | Right, displaced |
| S52.**2 | Left, displaced |
| S52.**4 | Right, nondisplaced |
| S52.**5 | Left, nondisplaced |
| S52.*1* | Greenstick |
| S52.*2* | Transverse |
| S52.*3* | Oblique |
| S52.*4* | Spiral |
| S52.*5* | Comminuted |
| S52.*6* | Segmental |
| S52.27* | Monteggia’s fracture of ulna |
| S52.37* | Galeazzi’s fracture of radius |
| S52.*8* | Bent bone |
| S52.*9* | Other |