Patella Dislocation
- A common athletic injury that frequently occurs in the youth
- Direct and indirect mechanisms of injury
- These dislocations frequently auto-reduce or are reduced by an athletic trainer prior to presentation
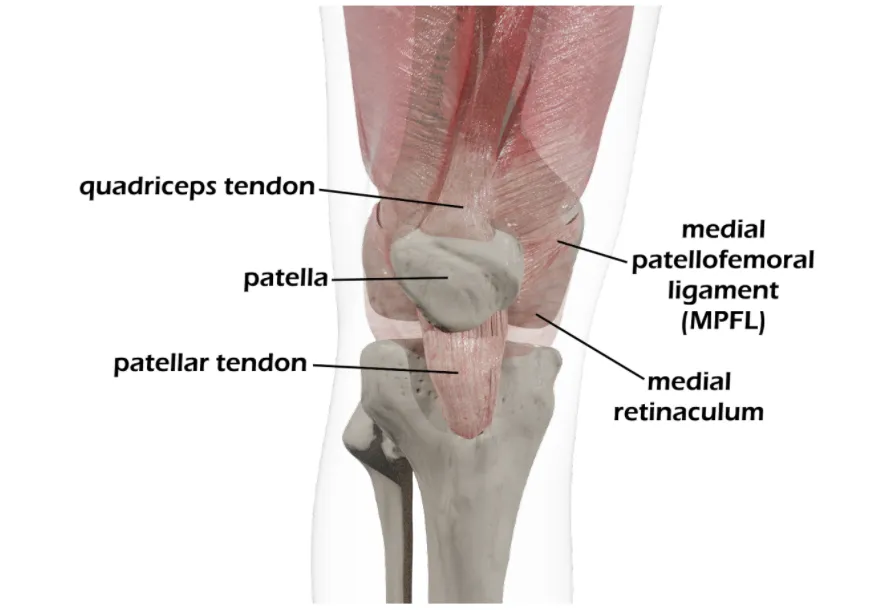
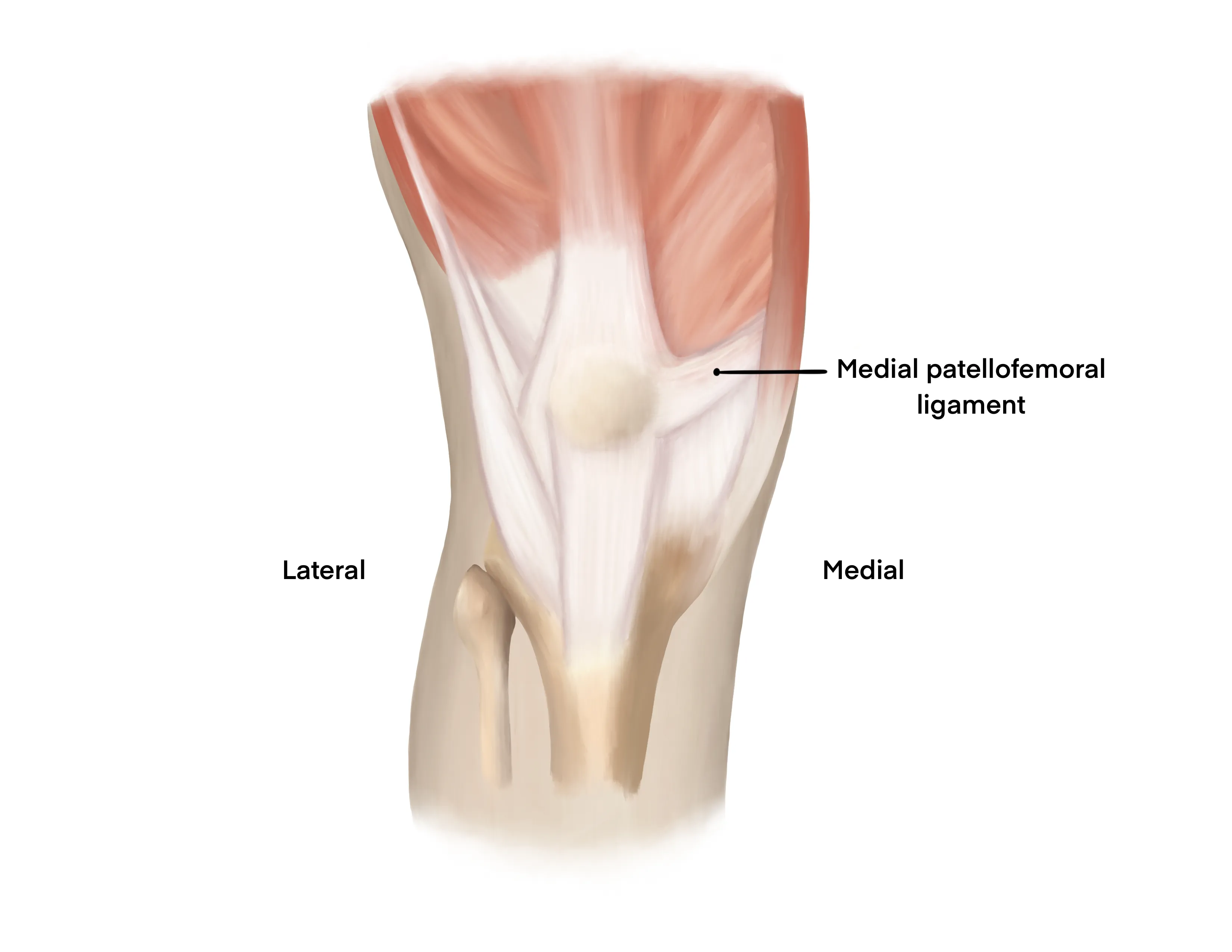
- If concerned for a dislocation event in a patient whose dislocation has been reduced, palpate over the medial patellofemoral ligament where point tenderness is often felt
- These patients can undergo closed reduction and application of a knee immobilizer
- Once reduced, the patient may be weightbearing-as-tolerated with the knee locked in extension (knee immobilizer) and crutches for assistance
- Orthopaedic follow up within 2 weeks
- Mechanism
- Commonly occurs in athletes
- Often a direct blow to the knee or indirect injury resulting from quadriceps contraction with leg in a valgus position
- Timing of injury
- Currently dislocated vs. reduced
- Often the dislocation auto-reduces or athletic trainers reduce it prior to presentation to the ED
- Parse out what happened at the time of injury
- Often will report the kneecap was displaced laterally to normal position
- Other locations of pain
- Numbness/tingling
- Prior dislocation events
- Implications on subsequent treatment (nonoperative vs. operative)
- Prior surgeries for patellar instability
Vitals
- Remove any splint/wrapping to view the foot
- Assess location of patella - is it dislocated or reduced
- Ecchymosis/bruising, swelling
- Scars from prior knee surgery
- Effusion
- Palpate broadly about the knee
- Assess for knee effusion during palpation about the patella
- Often tender to palpation over the medial patellofemoral ligament (MPFL)
-
Motor Exam:
- Tibialis Anterior - Dorsiflexion
- Gastroc/Soleus - Plantarflexion
- EHL/FHL - Extension/Flexion of the great toe
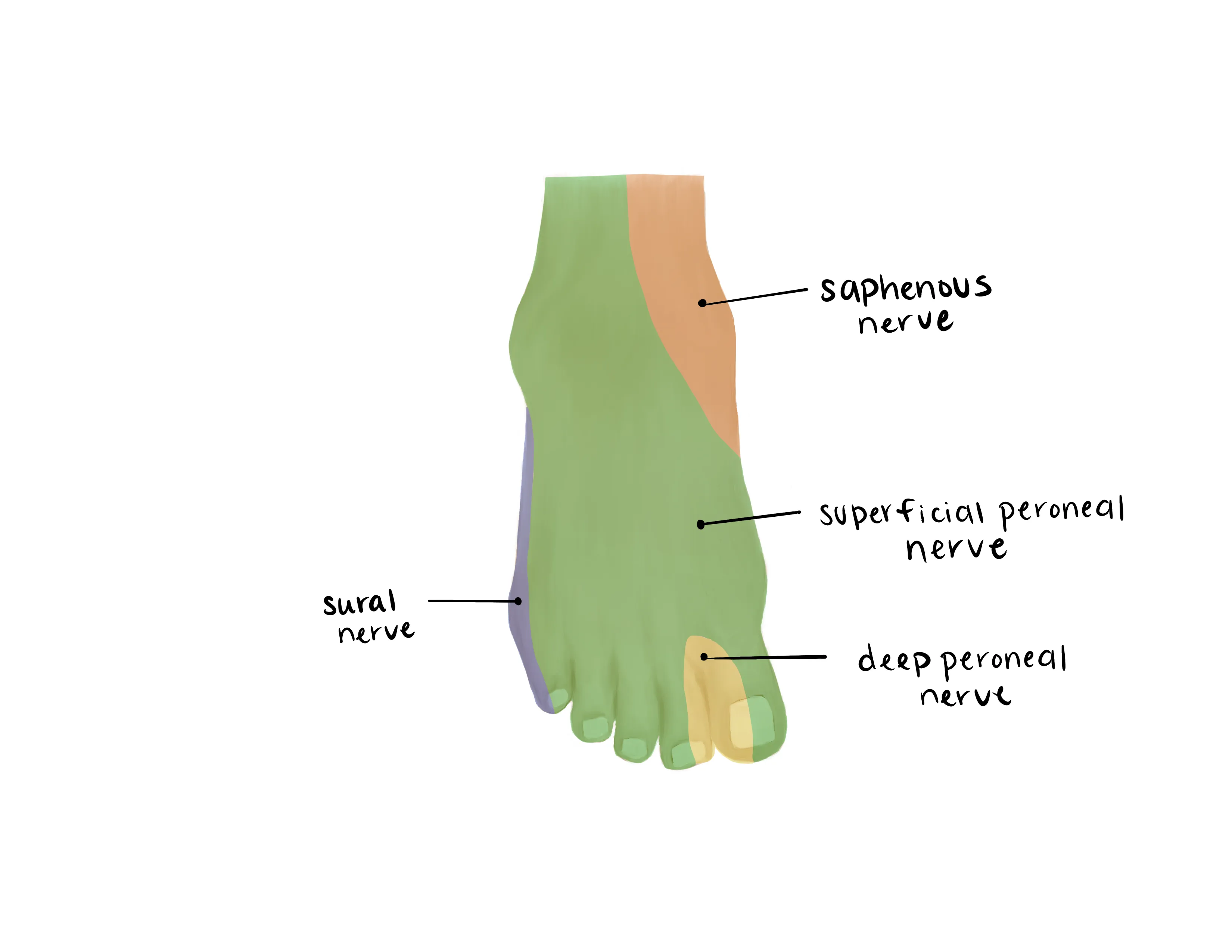
- Sural (Lateral)
- Saphenous (medial)
- Superficial Peroneal (dorsum)
- Deep Peroneal (1st web space)
- Tibial (plantar)
-
- Dorsalis Pedis/Posterior Tibial
- Capillary refill to toes
- If the patella remains dislocated, the patient will be unable to extend the knee
- If the patella is reduced, the patient may be able to range the knee but often has apprehension in doing so after injury
- Knee relaxed at ~30 degrees of flexion
- Apply laterally directed force to the medial patella
- Guarding and attempts to extend the leg indicate a positive test
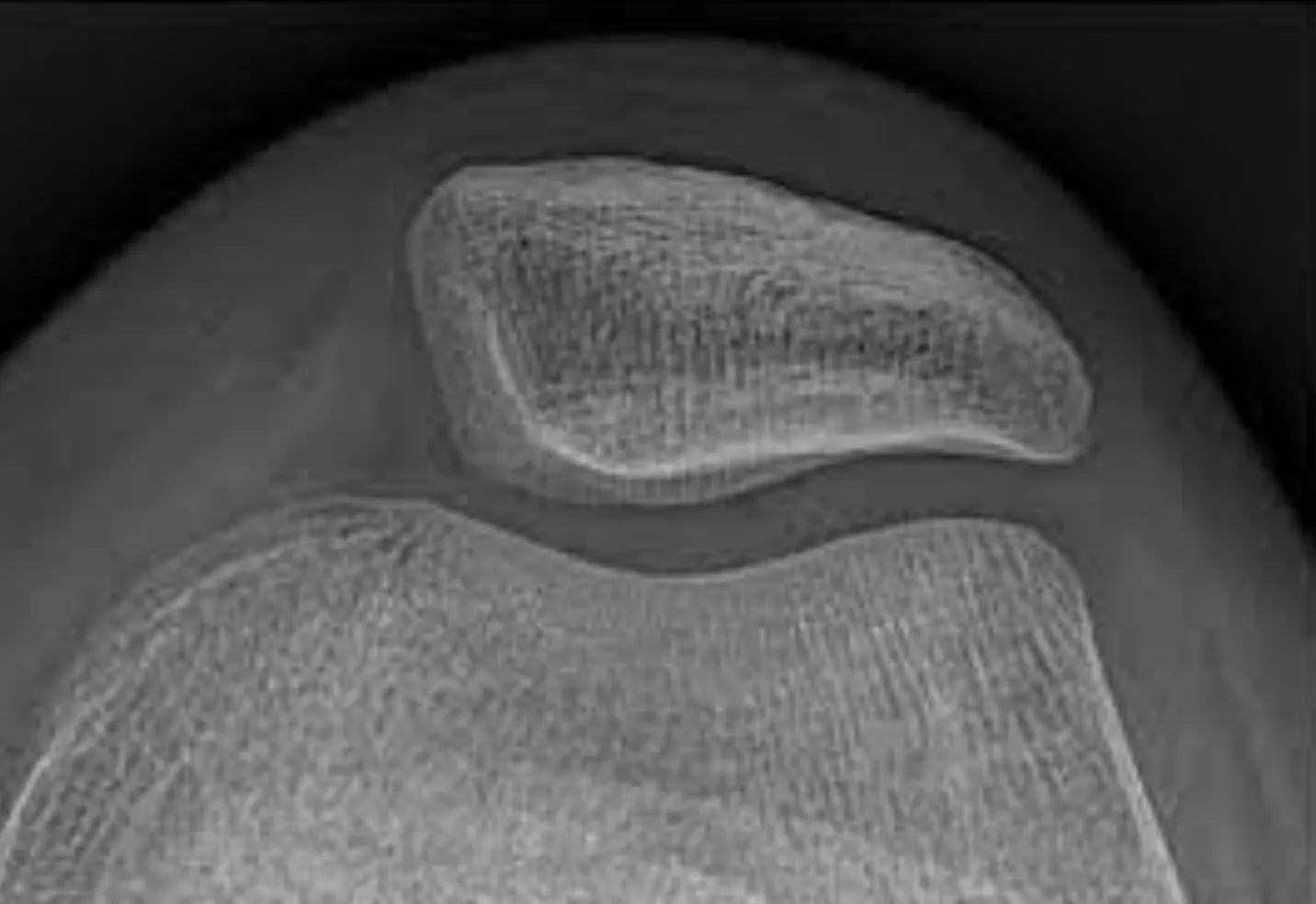
- AP/Lateral views of the femur and tibia; AP/Lateral/Sunrise view of the knee
- Rule out any concomitant fractures or injuries
- Obtain a sunrise view of the knee to ensure there is no patellar fracture
- CT scan - not needed in the ED
- May be obtained in the outpatient setting to assess tibial tubercle trochlear groove (TT-TG) distance for operative planning
- MRI - not needed in the ED
- May be obtained in the outpatient setting to assess soft tissue structures (MPFL, loose bodies, etc.)
Medical Decision Making
Dislocated Patella:
*** is a *** y/o ***M/F with a history of *** presenting with an injury to the ***R/L knee that occured while ***mechanism, found to have a patellar dislocation. The patient was neurovascularly intact and had no poke holes or lacerations that probed deep. Radiographs revealed ***. The patella was reduced and the patient was placed in a knee immobilizer to maintain the knee in full extension. Patient was provided crutches for comfort but may weightbear as tolerated and will follow up with orthopedic surgery 7-10 days for repeat evaluation.
Reduced Patella (Concern for dislocation event):
*** is a *** y/o ***M/F with a history of *** presenting with an injury to the ***R/L knee that occured while ***mechanism, believed to have had a patellar dislocation that reduced. The patient stated that at the time of injury, the patella was out lateral to its normal position and it ***autoreduced/was reduced by an athletic trainer. The patient was neurovascularly intact upon arrival and had no poke holes or lacerations that probed deep. Radiographs revealed ***. The knee was placed in a knee immobilizer to maintain the knee in full extension. Patient was provided crutches for comfort but may weightbear as tolerated and will follow up with orthopedic surgery 7-10 days for repeat evaluation.
Dislocated Patella:
- WB status: Weightbearing as tolerated with the injured lower extremity locked in extension with crutches for comfort (after reduction)
- Diet: Regular
- Analgesia: Short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 15 pills
- Immobilization:
- Closed reduction and application of knee immobilizer
- Disposition: Home with followup with orthopaedics in 1 week
- WB status: Weightbearing as tolerated with the injured lower extremity locked in extension with crutches for comfort
- Diet: Regular
- Analgesia: Short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 15 pills
- Immobilization:
- Knee immobilizer
- Disposition: Home with followup with orthopaedics in 1 week
Materials
Procedure Walkthroughs:
- Bring knee immobilizer into the room
- Provide the patient with IV/oral narcotics and anxiolytics for prophylactic analgesia
- Slowly begin to extend the knee
- As the patient begins to guard, apply a gentle lateral-to-medial directed force on the patella while continuing to extend the leg
- A palpable clunk is often felt as the patella reengages the trochlear groove
- Extend the knee into full extension and place in a knee immobilizer
- Bring knee immobilizer into the room
- Perform conscious sedation with appropriate staff in the room
- Slowly begin to extend the knee and apply a gentle lateral-to-medial directed force on the patella
- A palpable clunk is often felt as the patella reengages the trochlear groove
- Fully extend the knee into full extension and place in a knee immobilizer
Procedure Notes:
PROCEDURE NOTE: Closed treatment of patellar dislocation without anesthesia
PRE-PROCEDURE DIAGNOSIS: R/L*** Patellar dislocation
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: Oral/IV narcotics and anxiolytics***
NAME OF PROCEDURE: Closed treatment of patellar dislocation without anesthesia
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, stiffness, and inability to obtain reduction by closed means. Following informed verbal consent, after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
The knee was slowly extended with lateral to medial directed force over the patella. The patella reduced into the trochlea and then the knee came into full extension. The knee was placed in a knee immobilizer in extension. Neurovascular status was reassessed and was found to be consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharge with follow up with orthopaedic surgery within 7-10 days
PRE-PROCEDURE DIAGNOSIS: R/L*** Patellar dislocation
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: Oral/IV narcotics and anxiolytics***
NAME OF PROCEDURE: Closed treatment of patellar dislocation without anesthesia
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, stiffness, and inability to obtain reduction by closed means. Following informed verbal consent, after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
The knee was slowly extended with lateral to medial directed force over the patella. The patella reduced into the trochlea and then the knee came into full extension. The knee was placed in a knee immobilizer in extension. Neurovascular status was reassessed and was found to be consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharge with follow up with orthopaedic surgery within 7-10 days
PROCEDURE NOTE: Closed treatment of patellar dislocation with anesthesia
PRE-PROCEDURE DIAGNOSIS: R/L*** Patellar dislocation
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: Conscious sedation
NAME OF PROCEDURE: Closed treatment of patellar dislocation with anesthesia
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness, and inability to get the reduction by closed means. Following informed verbal consent, after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
The patient received conscious sedation with respiratory therapy present. Once the patient was adequately sedated, the knee was slowly extended with lateral to medial directed force over the patella. The patella reduced into the trochlea and then the knee came into full extension. The knee was placed in a knee immobilizer in extension. Neurovascular status was reassessed and was found to be consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharge with follow up with orthopaedic surgery within 7-10 days
PRE-PROCEDURE DIAGNOSIS: R/L*** Patellar dislocation
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: Conscious sedation
NAME OF PROCEDURE: Closed treatment of patellar dislocation with anesthesia
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness, and inability to get the reduction by closed means. Following informed verbal consent, after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
The patient received conscious sedation with respiratory therapy present. Once the patient was adequately sedated, the knee was slowly extended with lateral to medial directed force over the patella. The patella reduced into the trochlea and then the knee came into full extension. The knee was placed in a knee immobilizer in extension. Neurovascular status was reassessed and was found to be consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharge with follow up with orthopaedic surgery within 7-10 days
| Common ICD-10 Codes | Brief Description |
|---|---|
| S83.0 | Subluxation and dislocation of patella |
| S83.00 | Unspecified subluxation and dislocation of patella |
| S61.15 | Lateral subluxation and dislocation of patella |
| S61.3 | Other subluxation and dislocation of patella |
- Tintinalli, J. E., Stapczynski, J. S., Ma, O. J., Yealy, D. M., Meckler, G. D., & Cline, D. (2016). Injuries to Bones and Joints In Tintinalli's emergency medicine: A comprehensive study guide (Eighth edition.) (pp1863-1864). New York: McGraw-Hill Education.
- Davenport M. Procedures for orthopedic emergencies. In: Bond M, ed. Orthopedic Emergencies: Expert Management for the Emergency Physician. Cambridge: Cambridge University Press; October 31, 2013.
- Review of Orthopaedics, 6th Edition, Mark D. Miller MD, Stephen R. Thompson MBBS MEd FRCSC, Jennifer Hart MPAS PA-C ATC, an imprint of Elsevier, Philadelphia, Copyright 2012
- AAOS Comprehensive Orthopaedic Review, Jay R. Leiberman. Published by American Academy of Orthopaedic Surgeons, Rosemont IL. Copyright 2009
- Levy BA, Fanelli GC, Whelan DB, Stannard JP, MacDonald PA, Boyd JL, Marx RG, Stuart MJ. Knee Dislocation Study Group. Controversies in the treatment of knee dislocations and multiligament reconstruction. J Am Acad Orthop Surg. 2009 Apr;17(4):197-206. http://www.ncbi.nlm.nih.gov/pubmed/19307669
- Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, White LM. Epidemiology and natural history of acute patellar dislocation. AJSM 2004;32:1114-1121