Metacarpal Fracture
- General
- Metacarpal fractures are common hand fractures seen in the ED
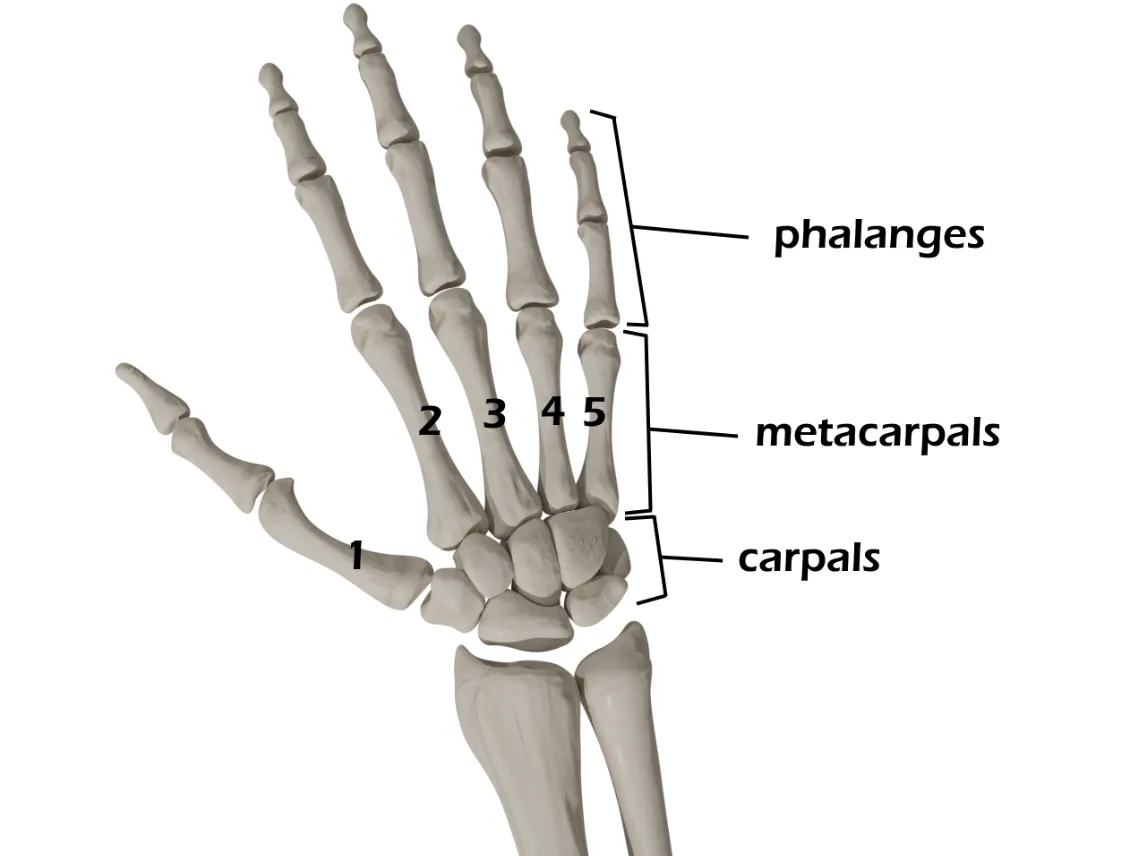
- Specific fracture patterns include:
- Bennett fracture - simple, intraarticular fracture of the base of the 1st (thumb) metacarpal
- Rolando fracture - comminuted, intraarticular fracture of the base of the 1st (thumb) metacarpal
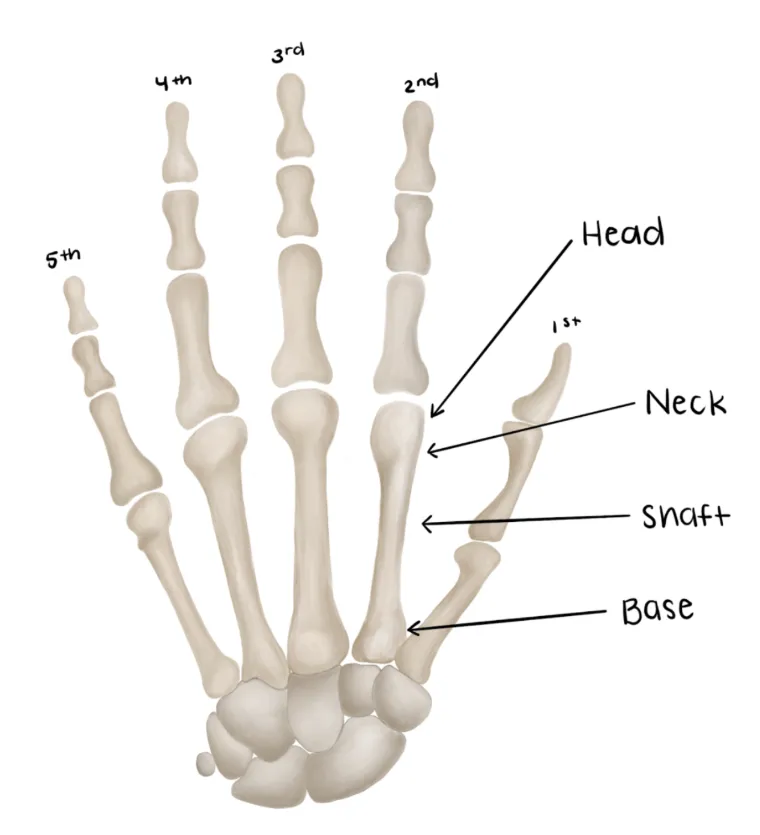
- Boxer’s fracture - angulated fracture at the neck of the 5th metacarpal
- Reverse Bennett fracture - intraarticular fracture of the base of the 5th metacarpal
- The hand should be examined for gross deformity, including malrotation and overlapping of digits when attempts are made to flex the digits (“scissoring”)
- Immobilization & WB Status
- Ulnar/Radial gutter splint +/- reduction
- Grossly aligned fractures should be splinted and referred to orthopaedics
- See parameters
- Grossly malaligned fractures should be reduced, splinted, and referred to orthopaedics
- Non-weight-bearing injured hand
- Disposition
- Open fractures require emergent orthopaedic consultation
- Closed fractures should follow up with orthpaedics in 1 week
- Mechanism
- Boxer’s fractures are usually the result of punching a hard object
- Timing of injury
- Other locations of pain/Associated injuries
- Numbness/tingling
- Hand dominance
- Profession
Vitals
- Swelling about the metacarpals
- Pain with palpation
- Poke holes or punctate wounds → open fracture
- Dorsal wounds are almost always open fractures
- Do not miss this and confirm 2-3g IV cefazolin was given
- Distal sensation on ulnar and radial side of the injured finger
- Two point discrimination
- Capillary refill
- Will likely be pain limited
- Extension of DIPJ, PIPJ, MCPJ, Wrist
- Extensor tendons can be lacerated
- Flexion of the DIPJ, PIPJ, MCPJ, Wrist
- AP/Lateral/Oblique of involved ray and hand
| Acceptable Shaft Angulation (degrees) | Acceptable Shaft Shortening (mm) | Acceptable Neck Angulation (degrees) | |
|---|---|---|---|
| Index & Long Finger | 10-20 | 2-5 | 10-15 |
| Ring Finger | 30 | 2-5 | 30-40 |
| Little Finger | 40 | 2-5 | 50-60 |
Medical Decision Making
Closed metacarpal fracture :
*** is a *** y/o ***R/L-hand dominant ***M/F with hx of *** who presents with an injury to the ***R/L hand which occurred while ***mechanism, found to have a ***1st-5th ***metacarpal fracture. On exam, the patient is neurovascularly intact with well perfused digits. The injury was closed with no poke holes or punctate wounds. Radiographs reveal ***. There ***was/was not malrotation of the digit when a fist was made. The fracture ***was/was not reduced and immobilized in a ***radial gutter/ulnar gutter/thumb spica splint. Post reduction XRs show improved alignment. The patient will follow up with orthopaedics/hand surgery within one week.
Open metacarpal fracture :
*** is a *** y/o ***R/L-hand dominant ***M/F with hx of *** who presents with an injury to the ***R/L hand which occurred while ***mechanism, found to have an open ***1st-5th metacarpal fracture. On exam, the patient is neurovascularly intact with well perfused digits. There was noted to be an ***cm laceration on the ***volar/dorsal surface of the hand which probes to fracture. Gross contaminants were irrigated from the wound at bedside. The patient was given an immediate dose of IV ***cefazolin/gentamicin. Orthopaedics was consulted and the patient was made NPO. Radiographs reveal ***. Orthopaedics to provide further recommendations.
If open fracture:
- Consult orthopaedic surgery
- NPO
- Ensure IV antibiotics were given (cefazolin vs. gentamicin)
- Gustillo-Anderson chart for antibiotic type and dose
- Diet: Regular
- Analgesia: short course of narcotic pain medication, acetaminophen (scheduled)
- Ex: 5mg oxycodone q4h - 15 pills
- Immobilization
- Ulnar/Radial Gutter or Thumb Spica +/- reduction (see procedures below)
- 1st metacarpal = thumb spica splint
- 2nd/3rd metacarpal = radial gutter splint
- 4th/5th metacarpal = ulnar gutter splint
- Assess angulation/displacement based on the parameters above
- If grossly aligned, hand should be splinted without reduction
- See acceptable parameters for nonoperative treatment in imaging section above
- If grossly malaligned, attempt closed reduction & splinting
- As always, if you feel uncomfortable with the reduction, consult orthopaedic surgery
- Disposition: Home with follow up in orthopaedic/hand surgery clinic in 1 week
Materials
Procedure Walkthroughs:
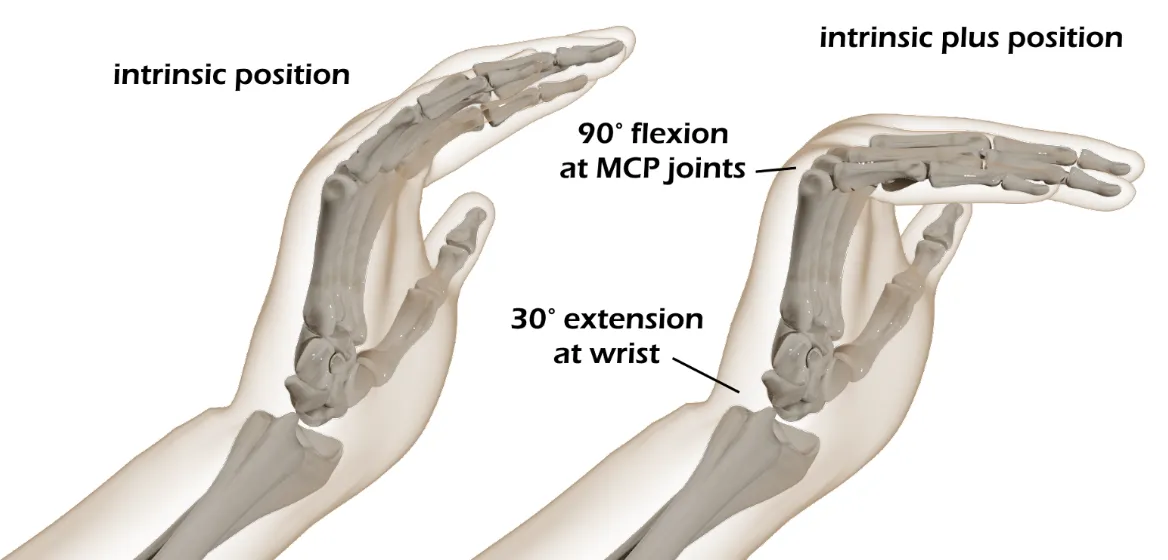
- Position: Wrist in 30 degrees of extension, MCP joints flexed 90 degrees, interphalangeal (IP) joints extended
- Apply soft padding liberally over forearm and ulnar digits (4th/5th digits)
- Measure plaster from the padding proximal to the wrist down to the distal extent of the padding on the small finger
- After wetting, use the plaster/orthoglass to sandwich the ulnar border digits coming from the ulnar side
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with preferred elastic or non-elastic bandage
- Wrist in 30 degrees of extension, MCP joints flexed 90 degrees, interphalangeal (IP) joints extended
- Apply soft padding liberally over forearm and the 2nd/3rd digits
- Measure plaster from padding proximal to the wrist down to the distal extent of the padding on the index finger
- Radial gutter splint should include a hemisphere cut out of the plaster at the level of the thumb to attempt to preserve thumb function
- After wetting, use the plaster/orthoglass to sandwich the 2nd/3rd border digits coming from the radial side
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with preferred elastic or non-elastic bandage
- Position: as if holding a can of soda
- Apply soft padding liberally over the thumb, wrist, and distal forearm
- Split/cut the plaster/orthoglass longitudinal with its length on one end
- After wetting, use the split end to cocoon the first ray with the hand in the position as if holding a can of soda
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with preferred elastic or non-elastic bandage
- Pain control with hematoma block, PO or IV analgesics
- Reduction
- Metacarpal Neck Fracture - Jahss Maneuver
-
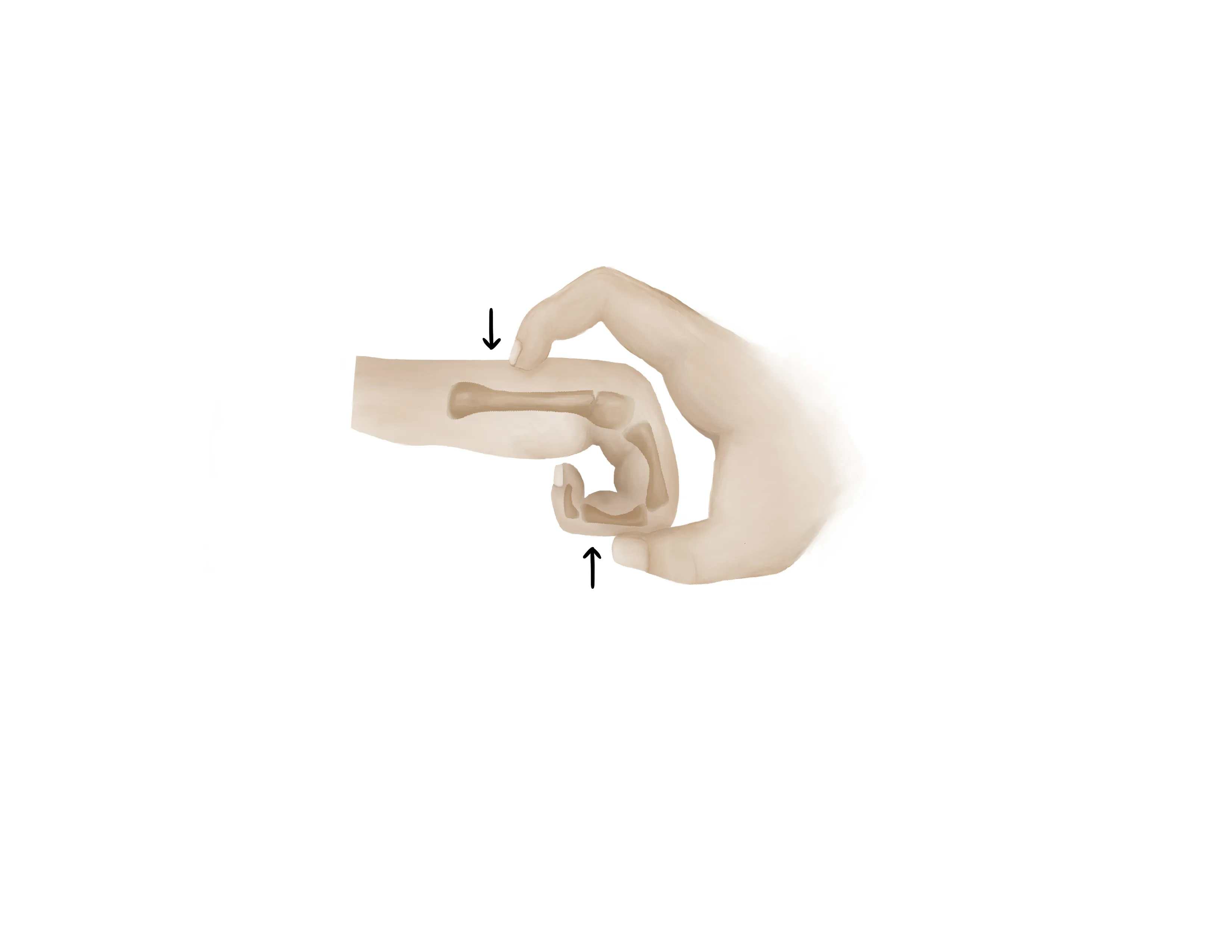
- Flex the MCPJ to 90 degrees
- Place dorsal pressure through the proximal phalanx when stabilizing the metacarpal shaft
- Metacarpal Shaft Fracture
- A combination of in line traction and pressure over the apex of the deformity can typically reduce these fractures
- Inherently stable and majority are minimally displaced
- Splinting
Procedure Notes:
PROCEDURE NOTE Closed treatment of 4th or 5th metacarpal fracture without manipulation
PRE-PROCEDURE DIAGNOSIS: fracture of the R/L*** *** metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of 4th or 5th metacarpal fracture without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
No attempt at reduction was made. An ulnar gutter splint was applied. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the R/L*** *** metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of 4th or 5th metacarpal fracture without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
No attempt at reduction was made. An ulnar gutter splint was applied. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE Closed treatment of 2nd or 3rd metacarpal fracture without manipulation
PRE-PROCEDURE DIAGNOSIS: fracture of the R/L*** *** metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of 2nd or 3rd metacarpal fracture without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
No attempt at reduction was made. A radial gutter splint was applied. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the R/L*** *** metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of 2nd or 3rd metacarpal fracture without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
No attempt at reduction was made. A radial gutter splint was applied. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE Closed treatment of 1st metacarpal fracture without manipulation
PRE-PROCEDURE DIAGNOSIS: Fracture of the R/L*** 1st metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of 1st metacarpal fracture without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, stiffness, numbness, and tingling. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
No attempts at reduction were made. A well-padded thumb spica splint was applied to the injured hand. Post splint radiographs showed unchanged alignment after the in-situ splinting. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: Fracture of the R/L*** 1st metacarpal
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of 1st metacarpal fracture without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, stiffness, numbness, and tingling. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
No attempts at reduction were made. A well-padded thumb spica splint was applied to the injured hand. Post splint radiographs showed unchanged alignment after the in-situ splinting. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE Closed Reduction and Splinting of the R/L*** *** metacarpal SHAFT fracture
PRE-PROCEDURE DIAGNOSIS: fracture of the *** metacarpal shaft
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV analgesia
NAME OF PROCEDURE: Closed Reduction and Splinting of the *** metacarpal shaft
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
After IV analgesia was administered.adequate time for analgesic effect was provided., The metacarpal shaft was reduced using a combination of traction and pressure over the apex of the deformity. Improvement in the gross deformity was observed.
A well-padded ***ulnar/radial gutter/thumb spica splint was then applied to the injured hand with care to maintain the hand in the intrinsic plus position. Post-reduction images showed improved alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** metacarpal shaft
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV analgesia
NAME OF PROCEDURE: Closed Reduction and Splinting of the *** metacarpal shaft
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
After IV analgesia was administered.adequate time for analgesic effect was provided., The metacarpal shaft was reduced using a combination of traction and pressure over the apex of the deformity. Improvement in the gross deformity was observed.
A well-padded ***ulnar/radial gutter/thumb spica splint was then applied to the injured hand with care to maintain the hand in the intrinsic plus position. Post-reduction images showed improved alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE Closed Reduction and Splinting of the R/L*** *** metacarpal NECK fracture
PRE-PROCEDURE DIAGNOSIS: fracture of the *** metacarpal neck
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV analgesia
NAME OF PROCEDURE: Closed Reduction and Splinting of the *** metacarpal neck
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
After IV analgesia was administered adequate time for analgesic effect was provided. The metacarpal neck was reduced using the Jahss maneuver.
A well-padded ***ulnar/radial gutter/thumb spica gutter splint was then applied to the injured hand with care to maintain the hand in the intrinsic plus position. Post-reduction images showed improved alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** metacarpal neck
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: IV analgesia
NAME OF PROCEDURE: Closed Reduction and Splinting of the *** metacarpal neck
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed. A timeout was performed.
After IV analgesia was administered adequate time for analgesic effect was provided. The metacarpal neck was reduced using the Jahss maneuver.
A well-padded ***ulnar/radial gutter/thumb spica gutter splint was then applied to the injured hand with care to maintain the hand in the intrinsic plus position. Post-reduction images showed improved alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
| Common ICD-10 Codes | Brief Description |
|---|---|
| S62.20 | Fracture of the first metacarpal bone, closed |
| S62.21 | Fracture of the first metacarpal bone, open |
| S62.30 | Fracture of other metacarpal bone, closed |
| S62.31 | Fracture of other metacarpal bone, open |
| S62.40 | Multiple fracture of metacarpal bones, closed |
| S62.41 | Multiple fracture of metacarpal bones, open |
- German C. Hand and wrist emergencies. In: Bond M, ed. Orthopedic Emergencies: Expert Management for the Emergency Physician. Cambridge: Cambridge University Press; October 31, 2013.
- Tintinalli, J. E., Stapczynski, J. S., Ma, O. J., Yealy, D. M., Meckler, G. D., & Cline, D. (2016). Injuries to Bones and Joints In Tintinalli's emergency medicine: A comprehensive study guide (Eighth edition.) (pp1863-1864). New York: McGraw-Hill Education.
- Davenport M. Procedures for orthopedic emergencies. In: Bond M, ed. Orthopedic Emergencies: Expert Management for the Emergency Physician. Cambridge: Cambridge University Press; October 31, 2013.


.webp?&w=600&h=600&fit=clip)