Jones and Pseudo-Jones Fractures
- 5th metatarsal base fractures are among the most common fractures of the foot
- Jones fractures occur at the metaphyseal-diaphyseal junction and, because of a tenuous blood supply, have a high rate of non-union
- Pseudo-Jones fractures are avulsion fractures of the tubercle and have better healing potential
- Proximal diaphyseal fractures (more distal than Jones fractures) also have a high rate of non-union
- Mechanism
- Jones fracture - twisting injury (adduction) of the forefoot
- Pseudo-Jones fracture - twisting injury (inversion) of the hindfoot
- Proximal diaphyseal fracture - often a stress fracture from repetitive microtrauma
- Timing of injury
- Missed injuries can lead to displacement and/or nonunion
- Other locations of pain
- Numbness/Tingling
- Profession
- Athletes at a higher risk of developing proximal diaphyseal stress fracture
- Increase in activity/training can often result in a stress fracture
- Tobacco use
- Poor healing potential
- Comorbidities
- Diabetes increases risk of nonunion and iatrogenic complications such as cast sores and ulcers
- Last time patient last ate (NPO status)
Vitals
- Gross appearance and palpation
- Swelling over the lateral foot
- Tenderness at the base of the 5th metatarsal
- Antalgic gait or refusing to bear weight
- Assess for poke hole/punctate wounds → open fracture
- Do not miss this and confirm antibiotics were given
- Motor
- Tibialis Anterior - Dorsiflexion
- Gastroc/Soleus - Plantarflexion
- EHL/FHL - Extension/Flexion of the great toe
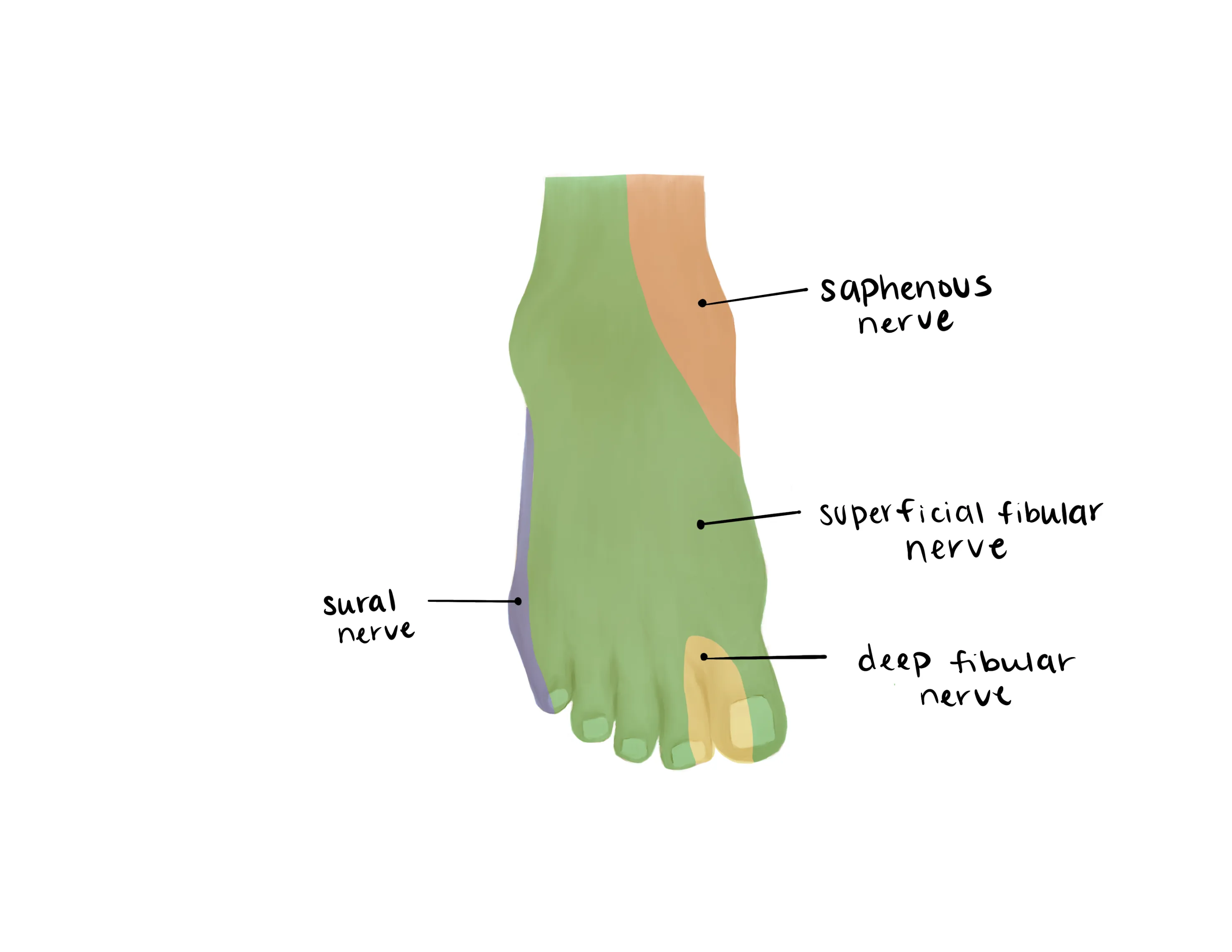
- Sensory (see image)
- Sural (Lateral)
- Saphenous(medial)
- Superficial Peroneal(dorsum)
- Deep Peroneal (1st web space)
- Tibial (plantar)
-
- Vascular exam:
- Dorsalis Pedis/Posterior Tibial
- Capillary refill to toes
- Dorsiflexion and plantar flexion at the ankle
- May be somewhat limited secondary to pain
- Toe flexion and extension
- May be limited secondary to pain at 4th and 5th toes
- Radiographs AP/lateral/oblique of involved foot
- Apophysis often mistaken for a fracture in children ages 10-16
- Apophysis has a longitudinal orientation along the metatarsal
-

- Avulsion fracture typically transverse
- Zone 1 - pseudo-Jones fracture; avulsion fracture of tubercle; typically heals well
- Zone 2 - true Jones fracture; high rate of non-union
- Zone 3 - proximal diaphysis; high rate of non-union
- MRI - not necessary in the ED
- Indicated for diagnosis of stress fractures not visible on plain film radiographs
- Edema in the bone represents stress reaction/fracture
- CT scan - not necessary in the ED
- May be indicated for more detailed evaluation if non-union suspected
- Occasionally helpful for preoperative planning
Medical Decision Making
*** is a *** y/o ***M/F with hx of ***, who presents with an injury to the *** lower extremity and concern for a 5th metatarsal fracture after mechanism***. On exam, the patient is neurovascularly intact. There is pain at the lateral border of the foot with tenderness at the 5th metatarsal base. The injury is closed and isolated. Radiographs reveal ***. The patient was placed in a ***CAM boot/well-padded short leg posterior splint] and instructed to remain nonweightbearing on the injured foot with crutches. The patient will ice and elevate the foot as needed and follow up with orthopedic surgery for further evaluation.
Open 5th metatarsal fracture:
- Consult orthopedics immediately
- NPO, preop labs (type and screen, INR, aPTT, CBC, BMP)
- Ensure IV antibiotics were given (ancef, gentamicin)
- Gustillo-Anderson chart for antibiotic type and dose
- WB Status: Nonweightbearing with crutches
- Caveat: small, non-displaced avulsion fractures (tubercle, pseudo-Jones) may weight bear in a CAM boot
- Diet: Regular
- Analgesia: short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 15 pills
- Immobilization: Short leg splint
- Caveat: small, non-displaced avulsion fractures (tubercle, pseudo-Jones) may weight bear in a CAM boot
- Disposition: Home with follow up in orthopedic clinic within 1 week
Materials for Splinting
Procedure Walkthroughs:
- Place patient’s leg in properly fitting boot, with heel securely fixed into the back of the boot
- Velcro the boot shut from the bottom to the top using the inner straps
- If there is a shield for the front of the boot, place it on the boot
- Velcro shut the outer straps of the boot from bottom to top
- Pump the boot so that the ankle is immobilized
- Position: Place the ankle in neutral position (do not splint in plantarflexion)
- Apply soft padding liberally over the foot and lower leg up to the level of the fibular head
- Apply extra padding at the malleoli of the ankle and the calcaneus
- Measure plaster/OrthoGlass plantarly from the level of the MTP joints, past the heel, on the posterior aspect of the leg to just distal to the popliteal fossa
- Measure plaster/OrthoGlass from just distal to the fibular head, down and around the heel, and up to the same level on the medial side
- Wet the plaster/Orthoglass pieces and apply them as they were measured taking care not to place any plaster directly on the skin
- Mold the splint about heel and malleoli while keeping the ankle at neutral
Procedure Notes:
PROCEDURE NOTE Closed treatment of metatarsal fracture; without manipulation
PRE-PROCEDURE DIAGNOSIS: R/L*** 5th metatarsal fracture
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of metatarsal fracture; without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
A well padded short leg splint was applied to the injured lower extremity with the ankle at neutral to keep the achilles on stretch and prevent contracture. The patient's neurovascular status was consistent with baseline after splint placement
COMPLICATIONS: ***
DISPOSITION: Discharged home with instruction to remain nonweightbearing on the injured extremity with elevation to reduce swelling. Follow up with orthopaedic surgery in 1 week.
PRE-PROCEDURE DIAGNOSIS: R/L*** 5th metatarsal fracture
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of metatarsal fracture; without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
A well padded short leg splint was applied to the injured lower extremity with the ankle at neutral to keep the achilles on stretch and prevent contracture. The patient's neurovascular status was consistent with baseline after splint placement
COMPLICATIONS: ***
DISPOSITION: Discharged home with instruction to remain nonweightbearing on the injured extremity with elevation to reduce swelling. Follow up with orthopaedic surgery in 1 week.
| Common ICD-10 Codes | Brief Description |
|---|---|
| S92.35 | Fracture of fifth metatarsal bone |
| S92.351 | Displaced fracture of fifth metatarsal bone, right foot |
| S92.352 | Displaced fracture of fifth metatarsal bone, left foot |
| S92.354 | Nondisplaced fracture of fifth metatarsal bone, right foot |
| S92.355 | Nondisplaced fracture of fifth metatarsal bone, left foot |



