Humeral Shaft Fracture
- Mechanism
- Usually a direct blow
- May occur from a fall on an outstretched arm in the elderly
- Timing of injury
- Other locations of pain
- Numbness or tingling
- Radial nerve palsy common with this type of injury
- Other fragility fracture (hip fx, compression fx of spine, proximal humerus fracture)
- Hand dominance
- Profession
- Possible implications on management
Vitals
- Remove wrapping or sling from about the shoulder/arm to assess the skin
- Assess for deformity, bruising, edema
- Soft tissue defect/poke hole that probes to fracture = open fracture
- Small poke hole wounds near the fracture site with a slow, continuous ooze is indicative of an open fracture
- Do not miss this and confirm antibiotics were given
- Do not forget to look in the axilla
- Examine the forearm compartments (soft and compressible, firm but compressible, etc.)
- Palpate the hand, wrist, elbow, arm and shoulder to identify concomitant injuries
- Palpate the compartments of the upper arm
- Compartment syndrome less common with humerus fractures but it is good to get a baseline assessment of the swelling
Motor Exam:
- Axillary nerve
- Difficult to assess because abduction will cause pain in this setting
- Backup: push elbow back into the bed/gurney
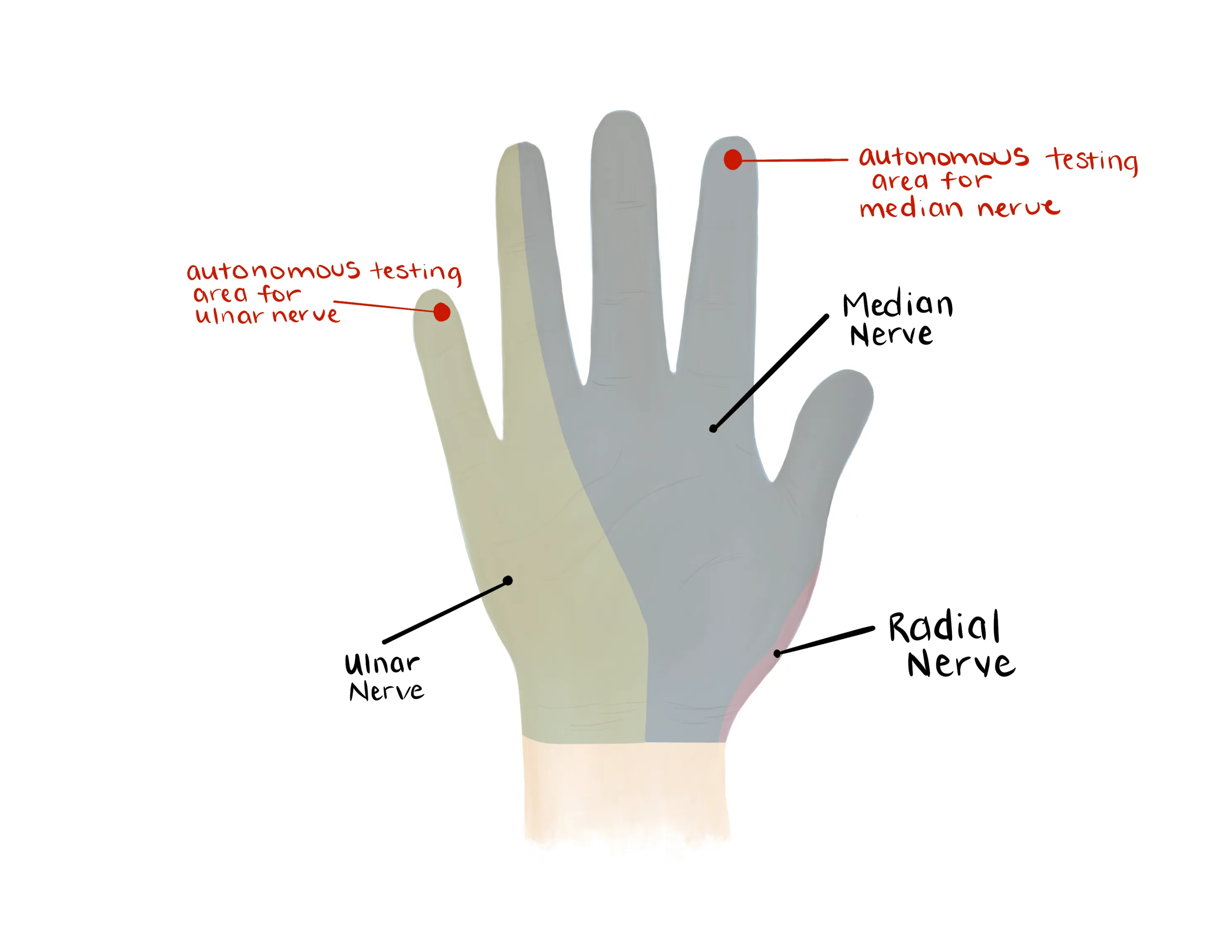
- Median Nerve/ Anterior interosseous nerve (AIN)
- Opposition of the thumb
- Opponens innervated by the median nerve - helpful to assess if concern for acute carpal tunnel syndrome
- Flexion of wrist, fingers, thumb
- “A-OK sign” = AIN
- Tests flexion of thumb IP joint (FPL) and flexion of index DIP joint (FDP)
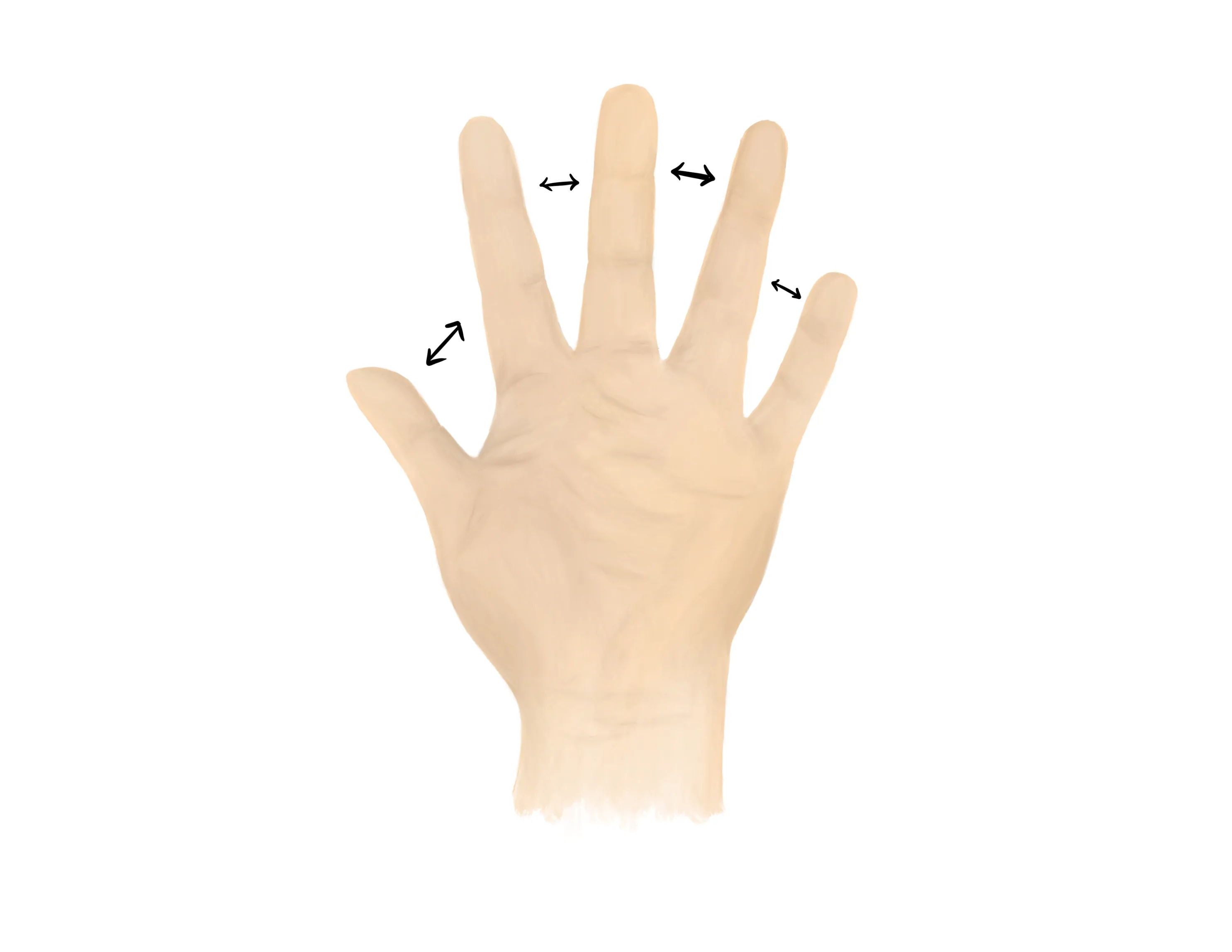
- Radial nerve/ Posterior interosseous nerve (PIN)
- Radial nerve palsy is commonly seen in humeral shaft fractures especially midshaft and distal third
-

- Extension of wrist, fingers, thumb
- Radial nerve palsy is common seen in humeral shaft fractures especially midshaft and distal third
- “Thumbs up” = PIN
- Tests extension of thumb IP and MCP joints (EPL))
- Palm on flat surface and lifting/extending thumb off the surface is also a good test for PIN (tests extension of thumb MCP joint (EPL))
- Ulnar nerve
- Median, Radial, Ulnar nerve distributions
- Radial artery, Ulnar artery
- If having difficulty with palpation of radial artery, find a US doppler
- Capillary refill to digits
- Limited ROM at the shoulder and elbow secondary to pain
- AP/Grashey/scapular Y and either axillary or Velpeau views of the shoulder, AP/lateral of the humerus, and AP/lateral of the elbow
- Key principle - joint above and below the fracture
- Axillary
- Beam directed into the axilla
- Requires patient to abduct which might be painful in the setting of proximal humerus fracture
-

- Velpeau
- Special views to consider:
- Traction view
- may be used for fractures with significant comminution, but not routinely indicated
- CT scan - not routinely obtained in the ED
Medical Decision Making
Closed humeral shaft fracture:
*** is a *** y/o ***R/L hand-dominant ***M/F with a history of *** presenting with an injury to the ***R/L arm that occured while ***mechanism, found to have a closed humeral shaft fracture. The patient had/did not have*** a radial nerve palsy. On exam, the injury was closed and there was normal capillary refill and a palpable radial pulse. Radiographs revealed ***. The arm was placed in a coaptation splint with a sling. The patient will follow up with orthopaedics in 7-10 days.
Open humeral shaft fracture:
*** is a *** y/o ***R/L hand-dominant ***M/F with a history of *** presenting with an injury to the ***R/L arm that occured while ***mechanism, found to have an open humeral shaft fracture. **IV antibiotics were given immediately upon presentation and tetanus prophylaxis/status was verified. The patient had/did not have*** a radial nerve palsy. There was a laceration that probed to fracture on the *** side of the arm. There was normal capillary refill and a palpable radial pulse. Radiographs revealed ***. Orthopaedics was consulted and will provide recommendations for further management. The patient was made npo and last ate ***.
If open fracture::
- Consult orthopaedic surgery immediately
- NPO, preop labs (type and screen, INR, aPTT, CBC, BMP)
- Ensure IV antibiotics were given (ancef, gentamicin)
- Gustillo-Anderson chart for antibiotic type and dose
- Consult orthopaedic surgery immediately
- NPO
- WB status: Nonweightbearing injured upper extremity
- Diet: Regular
- Analgesia: short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 25 pills
- Immobilization
- Coaptation splint and manipulation (vs. Sarmiento brace)
- If swelling or varus deformity, use coaptation splint
- If grossly angulated apply gentle force to straighten the humerus (typically valgus force)
- Generally important to place valgus mold on this splint
- These fractures fall into varus so applying a valgus mold helps decrease the risk of this
- If minimal swelling, may consider use of sarmiento brace
- Less common in the acute setting given swelling
- Disposition: Home with follow up in orthopedic surgery clinic in 7-10 days
Materials for Coaptation Splint
Procedure Walkthroughs:
- Apply soft padding over elbow, humerus, and shoulder to just above the acromioclavicular (AC) joint
- Measure plaster/Ortho-Glass from the axilla, around the elbow, and over the lateral surface of the deltoid
- Measure 5 layers of soft padding the length of the measured plaster/Ortho-Glass
- Wet the plaster/Ortho-Glass, place the 5 layers of soft padding underneath, and pass the plaster/Ortho-Glass and 5 layers of soft padding through large stockinette with long ends of stockinette on either side
- Place the plaster/Ortho-Glass/5 layers of soft padding/stockinette from the axilla, around the elbow, and over the lateral deltoid past the level of the shoulder if possible
- Use the long ends of the stockinette to wrap around contralateral shoulder and neck to help hold the plasters position
- Wrap the upper arm with an elastic bandage or wrap to further secure the splint
- Correct gross angulation of the humerus with gentle traction and pressure opposite the direction of angulation
- Apply soft padding over elbow, humerus, and shoulder to just above the acromioclavicular (AC) joint
- Measure plaster/Ortho-Glass from the axilla, around the elbow, and over the lateral surface of the deltoid
- Measure 5 layers of soft padding the length of the measured plaster/Ortho-Glass
- Wet the plaster/Ortho-Glass, place the 5 layers of soft padding underneath, and pass the plaster/Orthoglass and 5 layers of soft padding through large stockinette with long ends of stockinette on either side
- Place the plaster/Ortho-Glass/5 layers of soft padding/stockinette from the axilla, around the elbow, and over the lateral deltoid past the level of the shoulder if possible
- Use the long ends of the stockinette to wrap around contralateral shoulder and neck to help hold the plaster’s position
- Place a valgus mold about the fracture site to prevent the fracture from falling into varus
- Wrap the upper arm with elastic bandage or bias to further secure the splint
Procedure Notes:
PROCEDURE NOTE Closed treatment of humeral shaft fracture; without manipulation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** humerus
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of humeral shaft fracture; without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to radial nerve entrapment or paresthesias, post-procedural pain, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
A well-padded coaptation splint was applied to the injured extremity. A valgus mold was slowly applied as the splint hardened. Post splinting radiographs showed acceptable alignment after the splint application. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: None
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 7-10 days for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** humerus
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of humeral shaft fracture; without manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to radial nerve entrapment or paresthesias, post-procedural pain, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
A well-padded coaptation splint was applied to the injured extremity. A valgus mold was slowly applied as the splint hardened. Post splinting radiographs showed acceptable alignment after the splint application. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: None
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 7-10 days for repeat evaluation
PROCEDURE NOTE Closed treatment of humeral shaft fracture; with manipulation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** humerus
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of humeral shaft fracture; with manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to radial nerve entrapment or paresthesias, post-procedural pain, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
The angulation of the humerus was corrected with traction and gentle pressure opposite the direction of angulation. A well-padded coaptation splint was then applied to the injured extremity with a valgus mold as the splint hardened. Post manipulation radiographs showed improved alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: None
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 7-10 days for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** humerus
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of humeral shaft fracture; with manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to radial nerve entrapment or paresthesias, post-procedural pain, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
The angulation of the humerus was corrected with traction and gentle pressure opposite the direction of angulation. A well-padded coaptation splint was then applied to the injured extremity with a valgus mold as the splint hardened. Post manipulation radiographs showed improved alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: None
DISPOSITION: Discharged home with follow up with orthopaedic surgery in 7-10 days for repeat evaluation
| Common ICD-10 Codes | Brief Description |
|---|---|
| S42.3 | Fracture of shaft of humerus |
| S42.31 | Greenstick fracture of shaft of humerus |
| S42.32 | Transverse fracture of shaft of humerus |
| S42.33 | Oblique fracture of shaft of humerus |
| S42.34 | Spiral fracture of shaft of humerus |
| S42.35 | Comminuted fracture of shaft of humerus |
| S42.36 | Segmental fracture of shaft of humerus |