Distal Radius Fracture
- Fractures of the distal radius are some of the most common orthopaedic injuries seen in emergency departments
- Acute management:
- Nondisplaced/minimally displaced fractures can be splinted in-situ and discharged with orthopaedic follow up
- Displaced fractures should be reduced, immobilized in a sugar tong splint, and discharged with close orthopaedic follow up for possible outpatient intervention
- Complete a neurovascular exam before and after reduction
- If there is evolving paresthesias, pain, or lack of opposition - immediate consult to orthopaedics due to concern for acute carpal tunnel syndrome
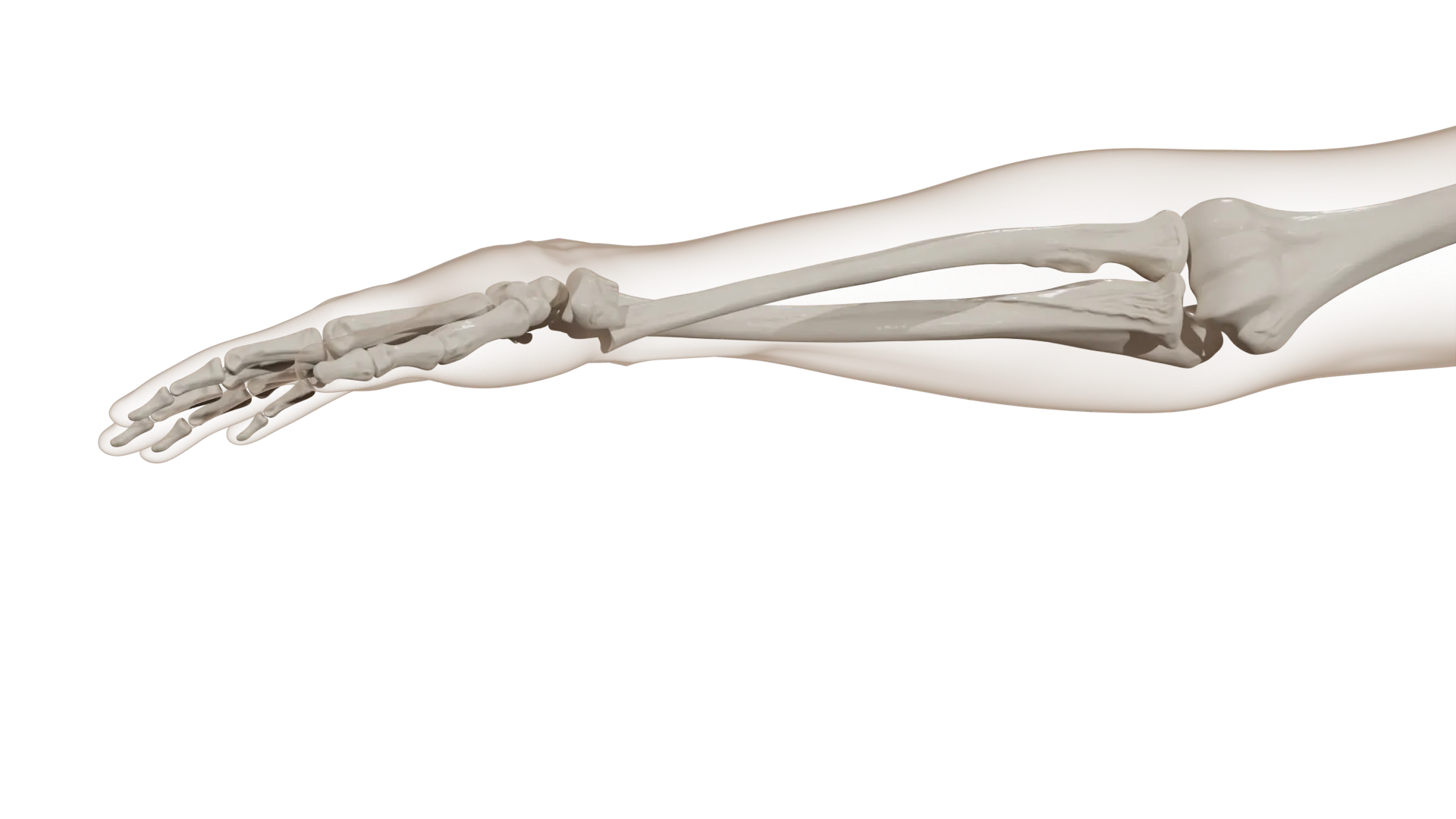
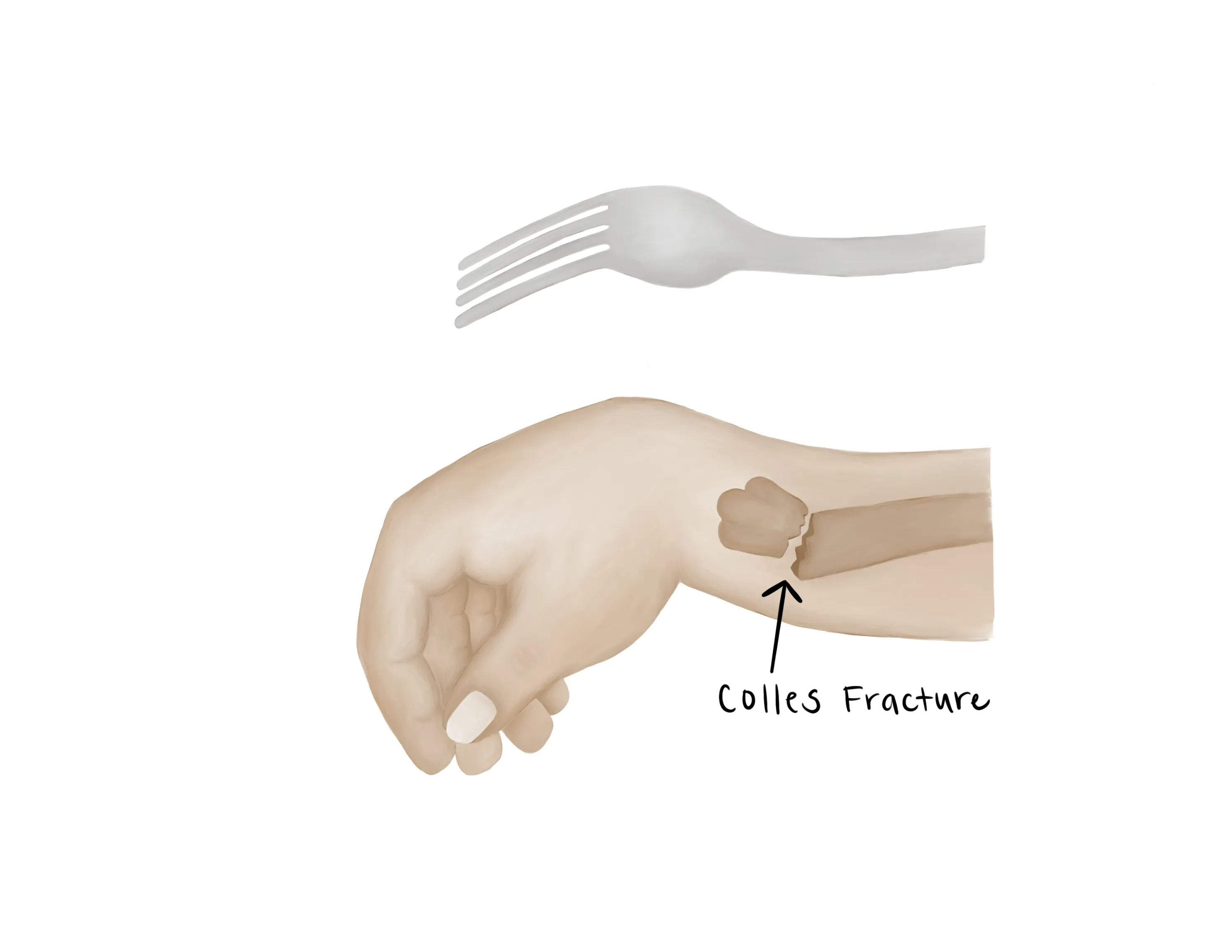
- Mechanism
- Often from a fall onto an outstretched arm, MVC, etc.
- Timing of injury
- Other locations of pain
- Palpate the entirety of the upper extremity to assess for concomitant injuries
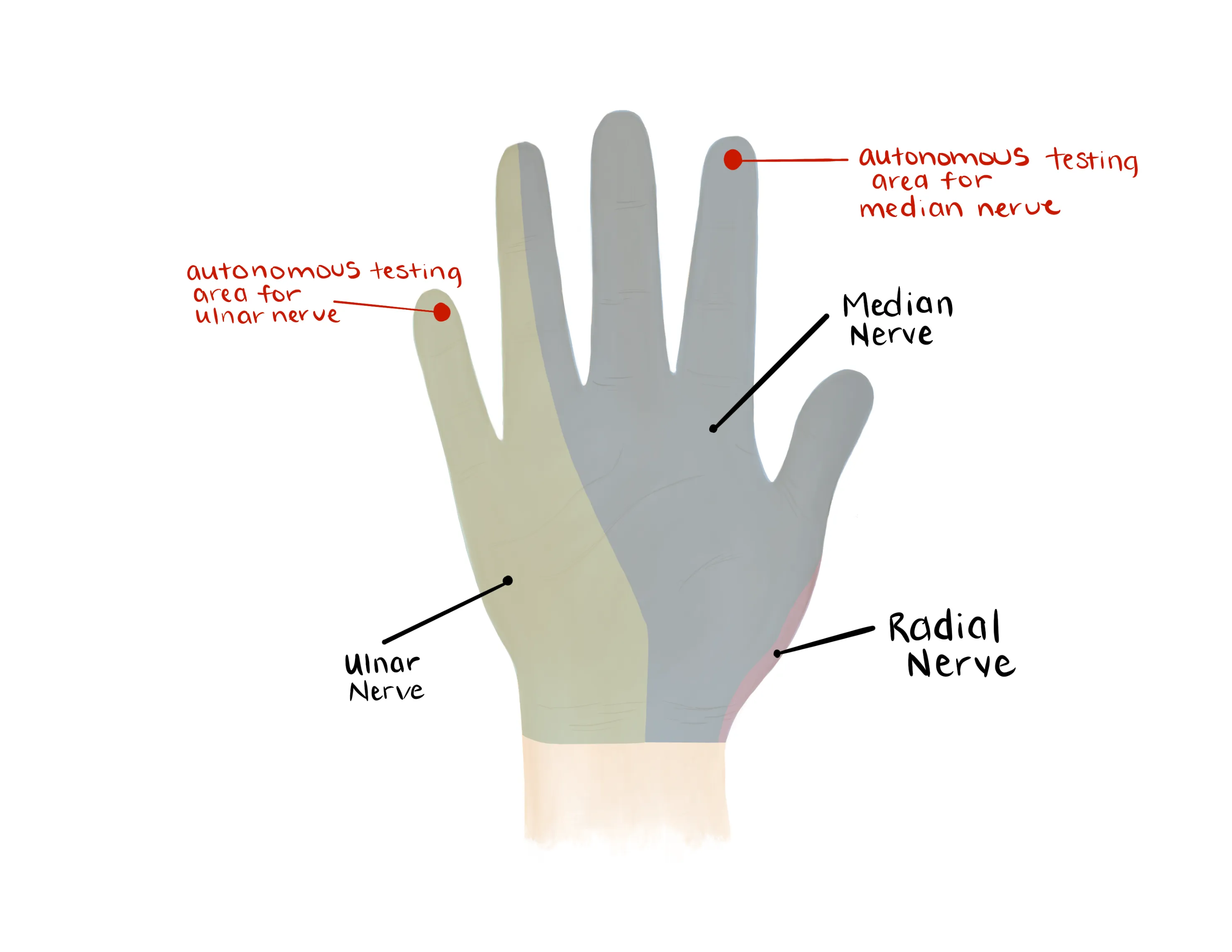
- Numbness or tingling and pain in median nerve distribution (see physical exam)
- Be wary of acute carpal tunnel syndrome
- Progressively worsening numbness/tingling/pain in median nerve distribution → requires urgent decompression
- Urgent consult to orthopaedic surgery
- Hand dominance (right vs. left hand dominant)
- Profession
- Nonoperatively managed fractures require longer immobilization than operatively managed fractures - often patients will opt for surgery for earlier mobilization
- Other fragility fracture (hip fracture, compression fracture of spine, proximal humerus fracture)
- Often DRF is a sentinel event before a more serious osteopenic/osteoporotic related fracture in the elderly such as a hip fracture
- Anticoagulation
- Last dose?
- Last time the patient ate (NPO status)
Vitals
- Gross appearance of the forearm (deformity, soft tissue defect, pokeholes)
- Soft tissue defect/poke hole that probes to fracture = open fracture
- Small poke hole wounds near the fracture site with a slow, continuous ooze is indicative of an open fracture
- Do not miss this - confirm 2-3g IV cefazolin was given
- Examine the forearm compartments
- Soft and compressible, firm but compressible, etc.
- Compartment syndrome is less common with distal fractures but should still be considered
- Palpate the hand, elbow, arm and shoulder to identify concomitant injuries
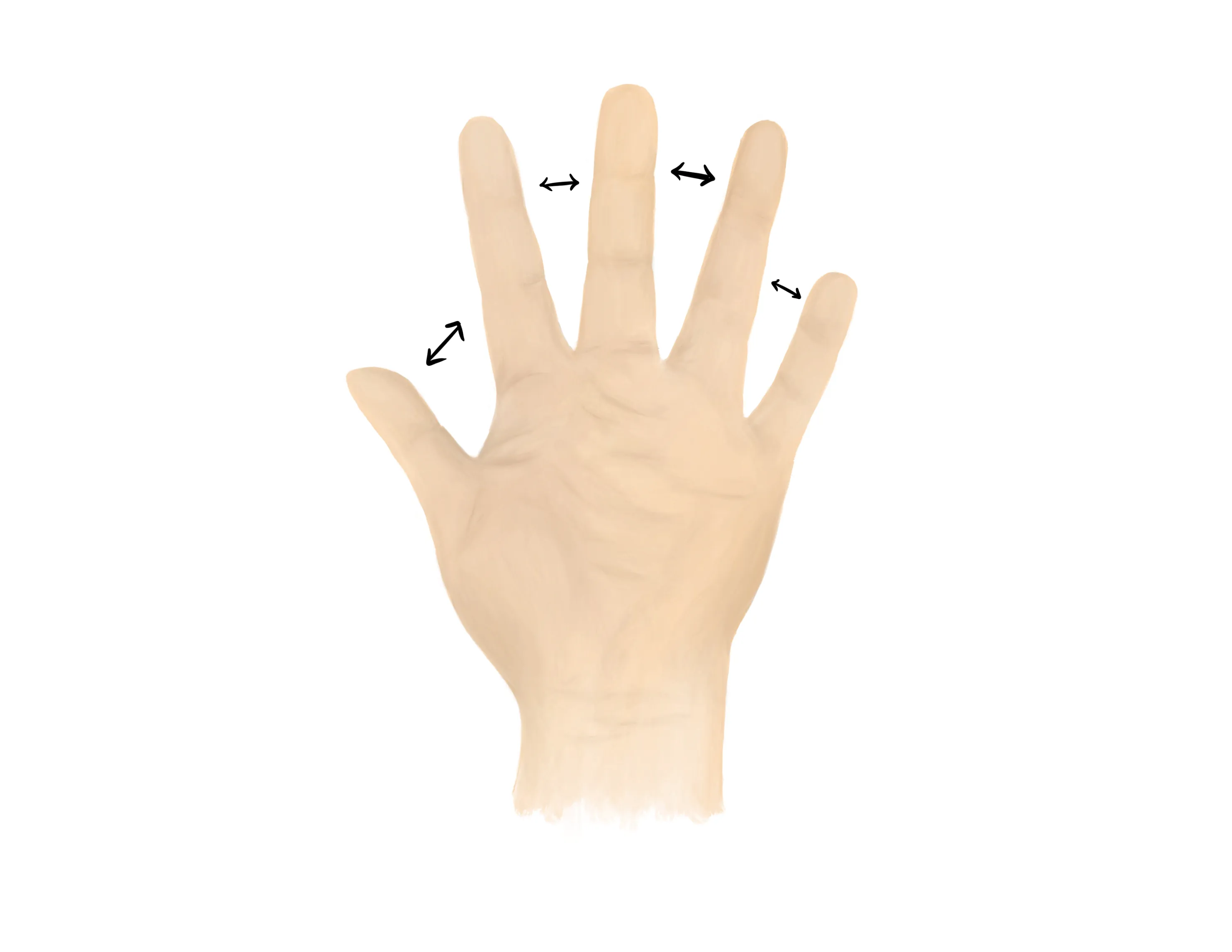
Motor Exam:
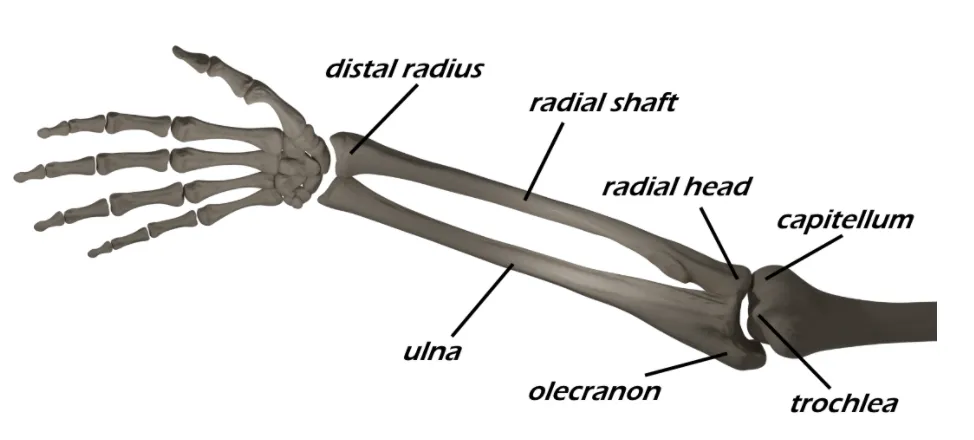
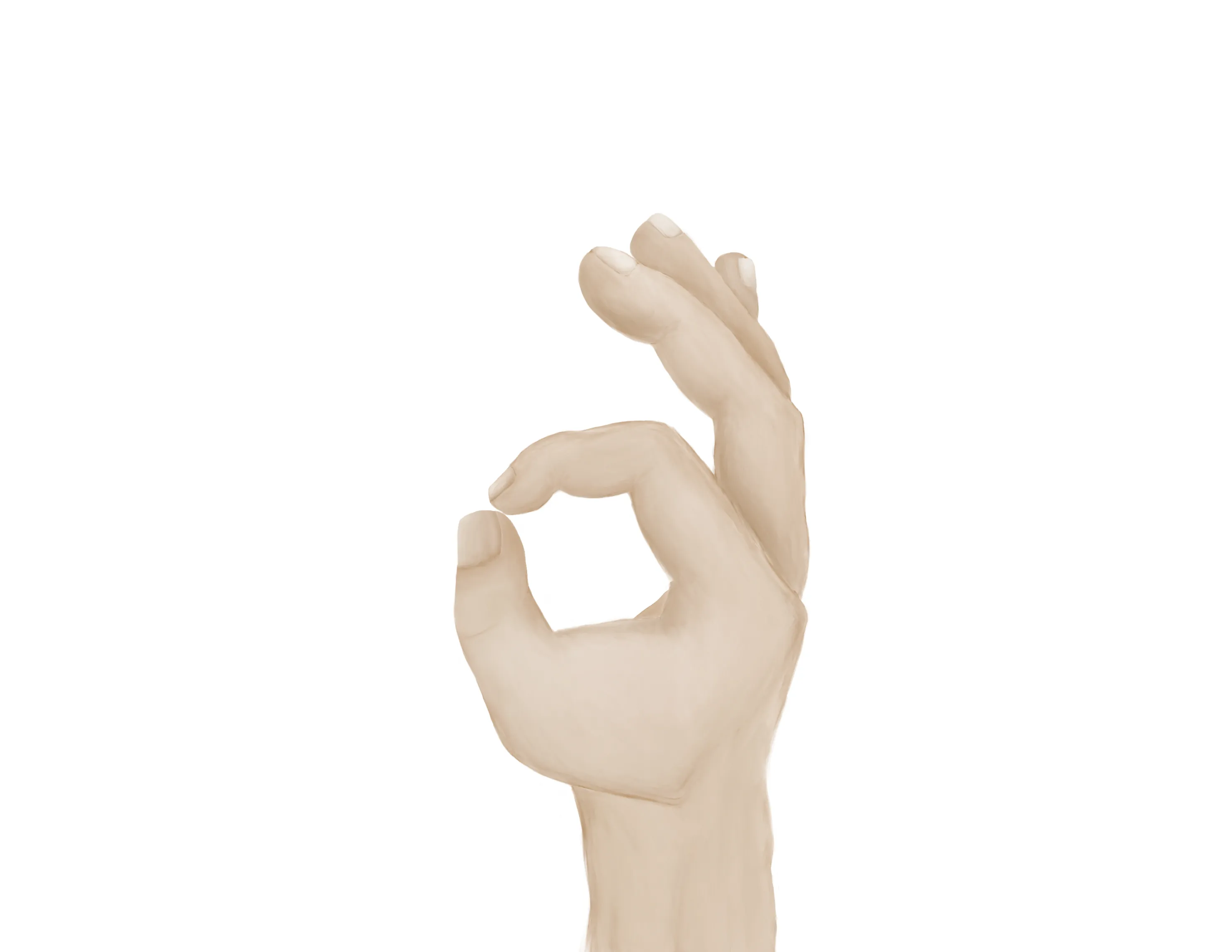
- Median Nerve/ Anterior interosseous nerve (AIN)
- Opposition of the thumb
- Opponens innervated by the median nerve - helpful to assess if concern for acute carpal tunnel syndrome
- Flexion of wrist, fingers, thumb
- “A-OK sign” = AIN
- Tests flexion of thumb IP joint (FPL) and flexion of index DIP joint (FDP)
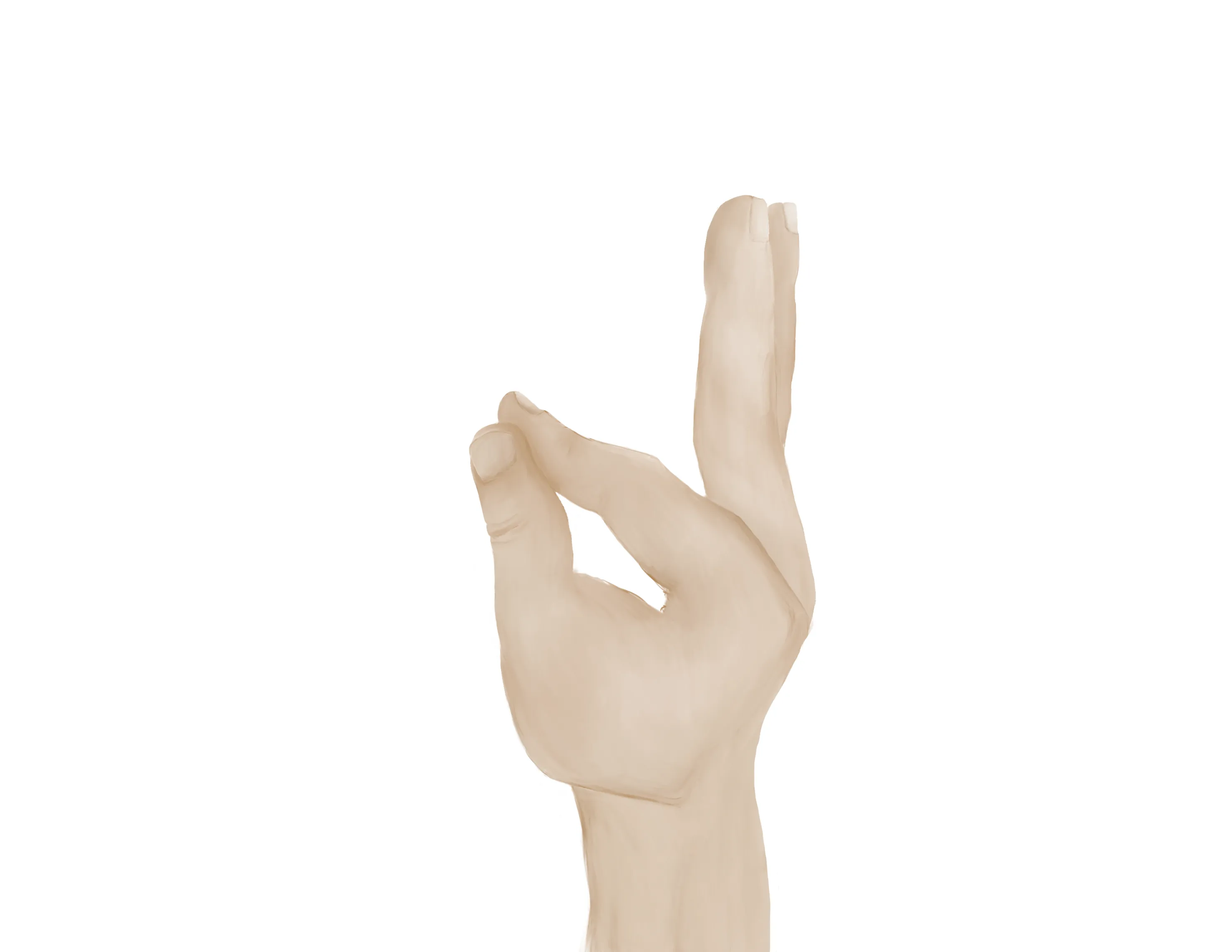
- Radial nerve/ Posterior interosseous nerve (PIN)
-

- Extension of wrist, fingers, thumb
- “Thumbs up” = PIN
- Tests extension of thumb IP and MCP joints (EPL))
- Palm on flat surface and lifting/extending thumb off the surface is also a good test for PIN (tests extension of thumb MCP joint (EPL))
- Ulnar nerve
- Median, Radial, Ulnar nerve distributions
- Radial artery, Ulnar artery
- If having difficulty with palpation of radial artery, find a US doppler
- Capillary refill to digits
- ROM at the wrist will likely be limited by pain
- AP/Lateral wrist, AP/Lateral radius & ulna, AP/Lateral elbow
- CT scan - rarely needed in the ED
- May be ordered by orthopaedics for preoperative planning if significant comminution and intraarticular extension
- Unlikely to change acute management
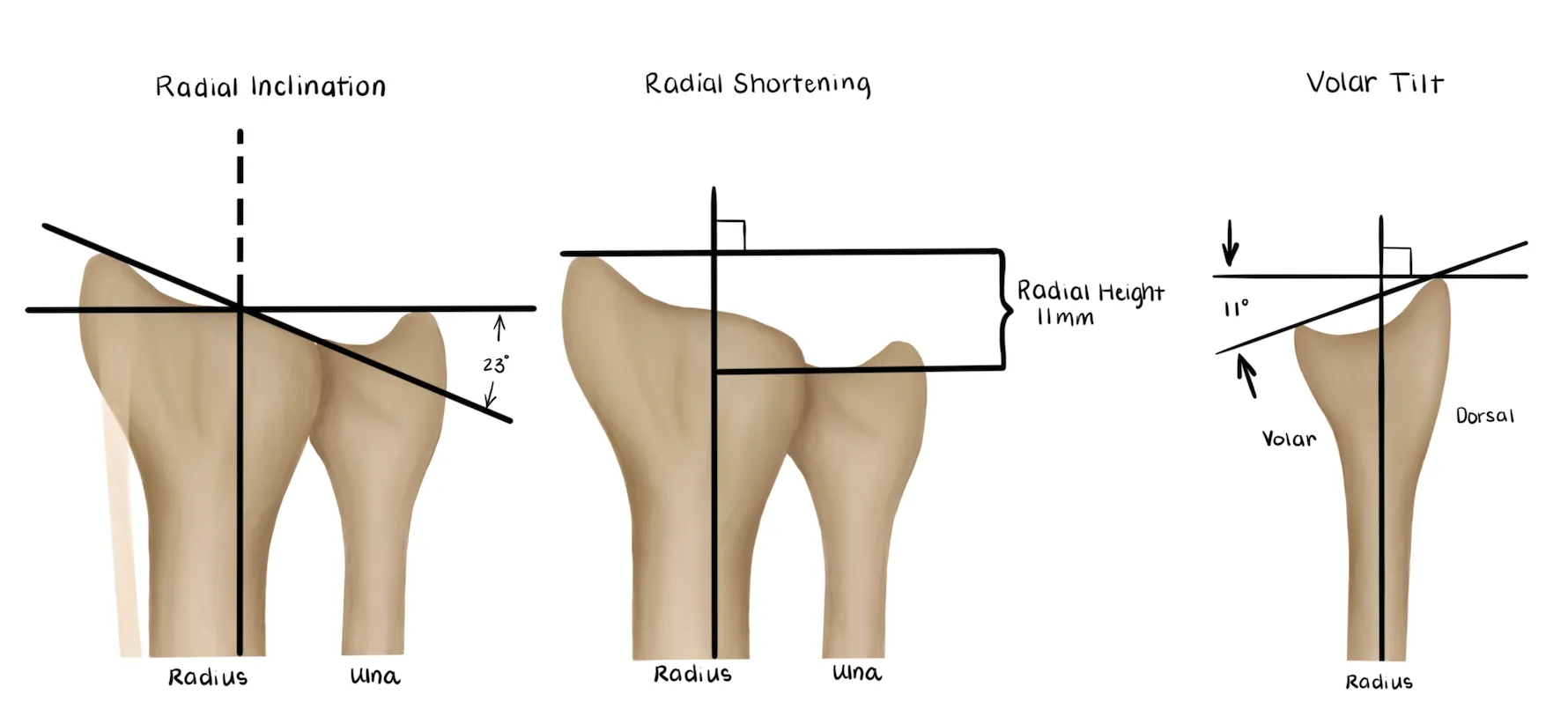
Normal parameters and acceptable criteria for nonoperative management:
| Normal | Acceptable criteria | |
|---|---|---|
| Radial Height (AP) | 13mm | < 5 mm shortening |
| Radial inclination (AP) | 23° | Change < 5° |
| Articular stepoff (AP) | Congruous | < 2 mm stepoff |
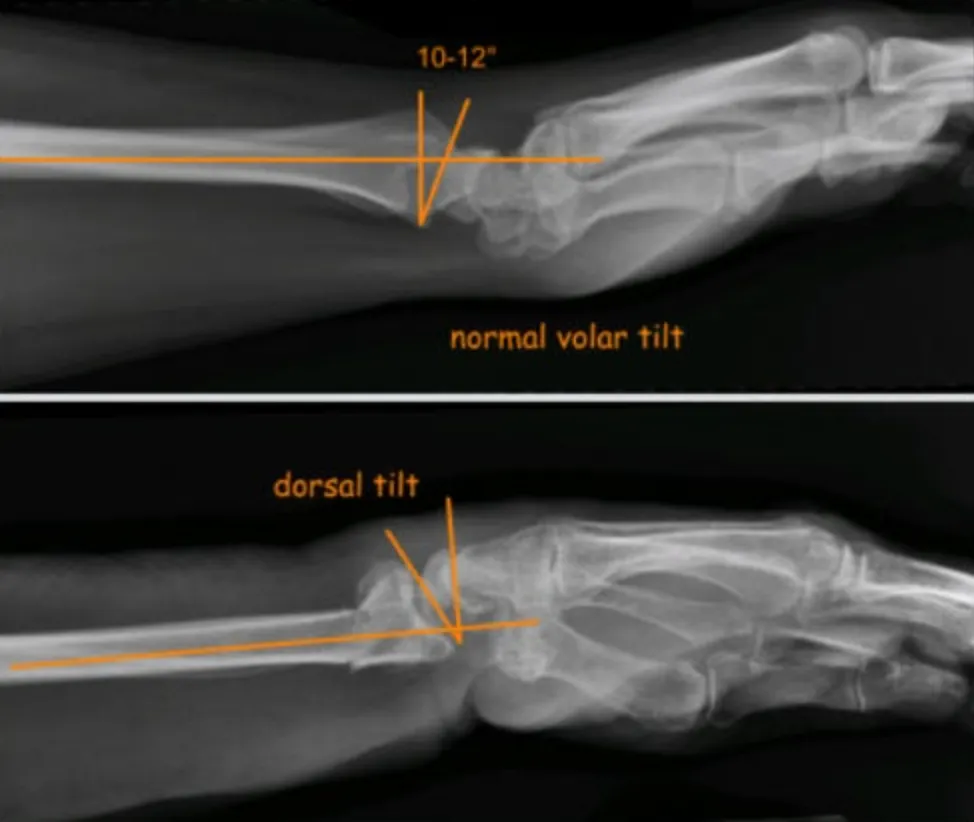
| Volar tilt (Lateral) | 11° | Dorsal angulation < 5° or within 20° of contralteral distal radius |
Medical Decision Making
Closed Distal Radius Fracture:
*** is a *** y/o ***R/L hand-dominant ***M/F with a history of *** presenting with an injury to the *** wrist which occurred while ***, found to have a closed distal radius fracture. On exam, the patient is neurovascularly intact with no poke holes or punctate wounds. There is tenderness to palpation and localized edema about the fracture site. Radiographs reveal ***. The fracture was/was not *** reduced and the patient was immobilized with a sugar tong splint and will follow up with orthopaedic surgery in one week.
Open Distal Radius Fracture
*** is a *** y/o ***R/L hand-dominant ***M/F with a history of *** presenting with an injury to the *** forearm which occurred while ***mechanism, found to have an open distal radius fracture. On exam, the patient is neurovascularly intact with an ***cm open wound on the ***location on wrist. The patient was immediately given a dose of IV ancef/gentamicin***. Radiographs reveal ***. Orthopaedics was consulted and the patient was kept NPO. Orthopaedic surgery to provide further recommendations.
Distal Radius with Concern for Acute Carpal Tunnel
*** is a *** y/o ***R/L hand-dominant ***M/Findividual with a history of *** presenting with an injury to the *** wrist which occurred while ***, found to have a closed distal radius fracture. On exam, the patient had tenderness to palpation about the wrist with paresthesia in the distribution of the median nerve and difficulty with opposition which has been getting worse since the time of injury. Radiographs reveal ***. Orthopaedics was immediately consulted for concern for acute carpal tunnel syndrome.
Open fracture or traumatic arthrotomy:
- Consult orthopaedic surgery immediately
- NPO
- Ensure IV antibiotics were given (cefazolin, gentamicin)
- Gustillo-Anderson chart for antibiotic type and dose
- Consult orthopaedic surgery immediately
- NPO
- Do not attempt reduction in this setting
- WB status: Nonweightbearing injured upper extremity
- Diet: Regular
- Analgesia: Short course of narcotic pain medication, tylenol (scheduled)
- Ex: 5mg oxycodone q4 - 25 pills
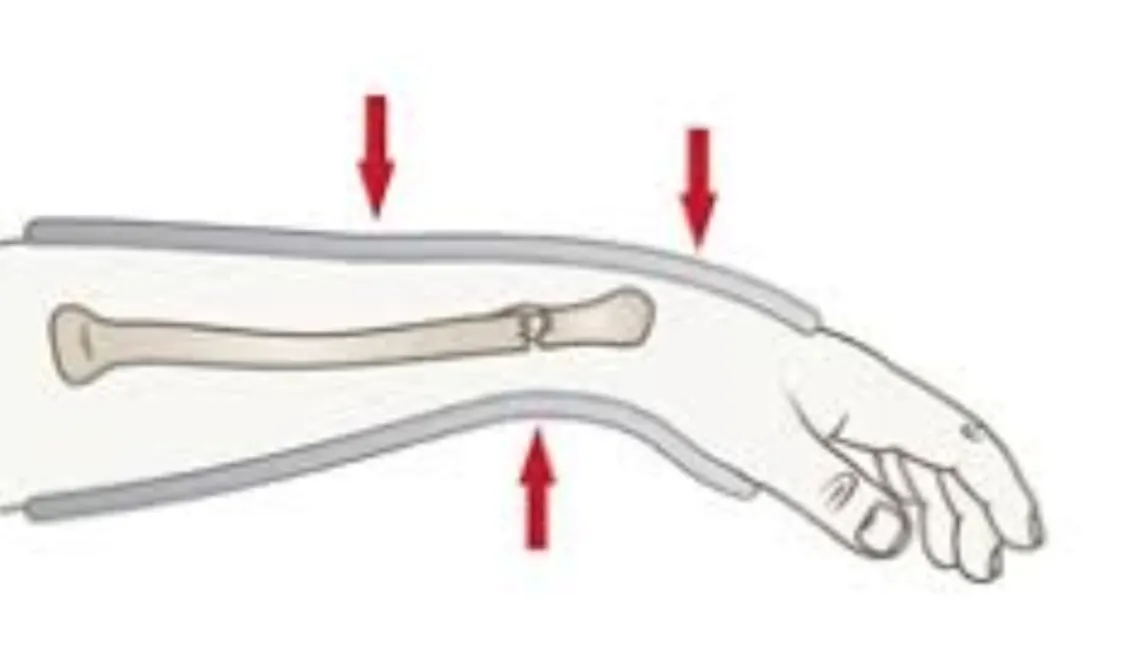
- Immobilization
- Sugar Tong Splint +/- reduction
- Assess angulation/displacement based on the parameters above
- If grossly aligned and minimally displaced, the forearm should be splinted without reduction (in-situ)
- If grossly malaligned with significant displacement based on above radiographic parameters (see imaging), attempt closed reduction & splinting
- As always, if you feel uncomfortable with the reduction, consult hand/orthopaedic surgery
- Disposition: Home with follow up in orthopaedic surgery clinic within 1 week
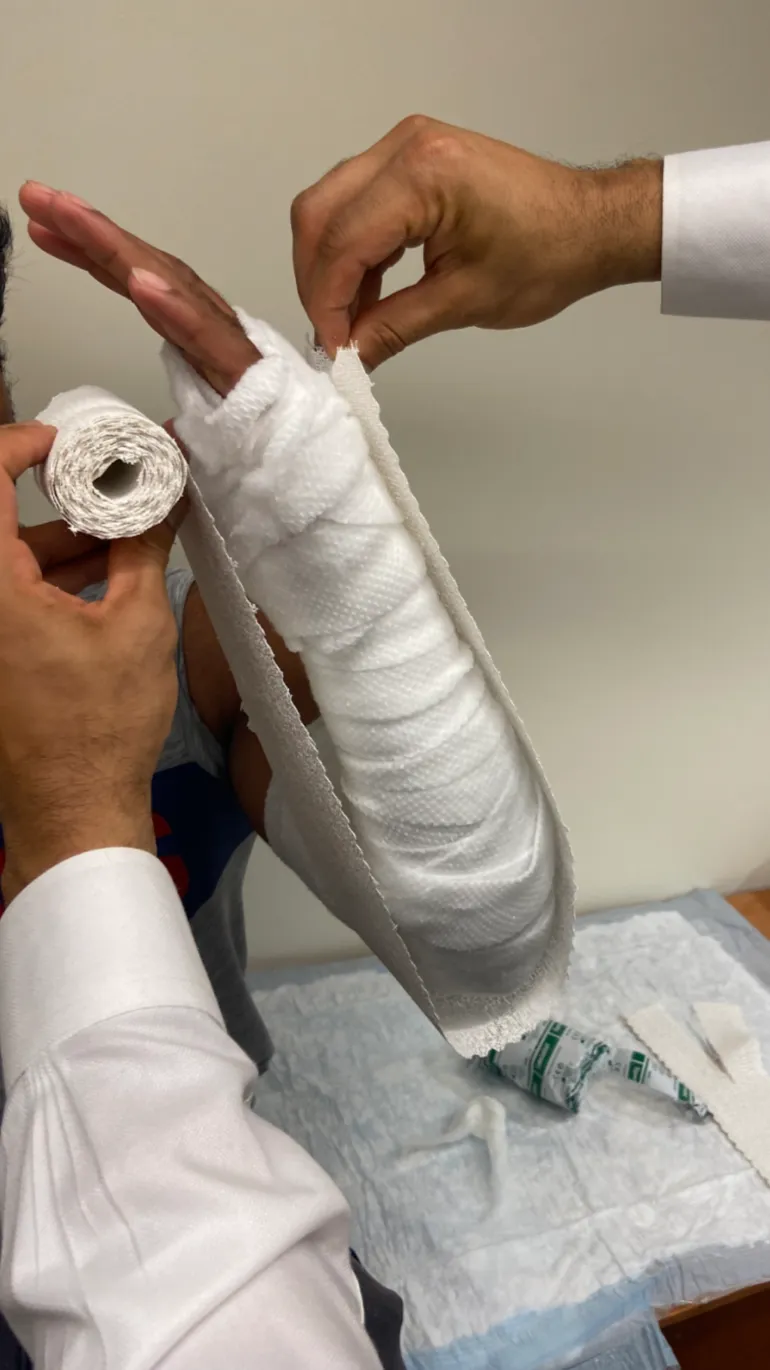
Materials
Procedure Walkthroughs:
- Apply soft padding liberally over elbow, forearm, and palm up to the level of the distal palmar crease
- Measure plaster/Ortho-Glass from the mid-palm over the volar surface of the forearm, around the elbow, and over the dorsal surface of the forearm to the same level distally
- After wetting, lay the plaster/Ortho-Glass from the mid-palm over the volar surface of the forearm, around the elbow, and over the dorsal surface of the forearm to the same level distally.
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with preferred elastic or non-elastic bandage.
- Perform hematoma block into the fracture site with 1% lidocaine with or without epinephrine and 0.25% bupivacaine (alternative is conscious sedation)
- Use c-arm (fluoroscopic) guidance to perform this since it will be needed for the reduction thereafter
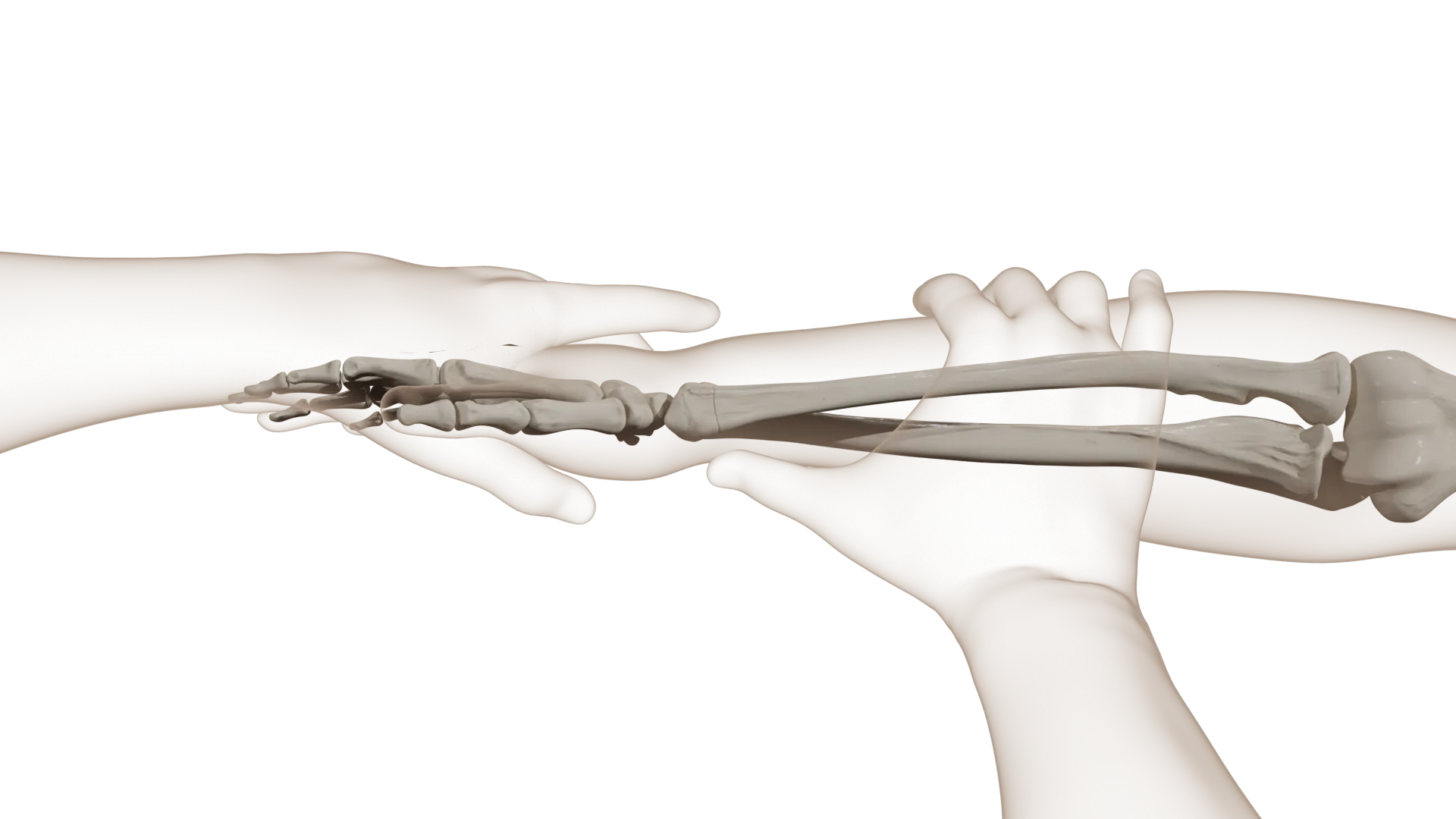
- Hang the extremity in traction/countertraction (institution dependent)
- Helps get length in fractures with shortening from the brachioradialis
- Get splint materials for a sugar tong splint, mini-C arm, lead
- Fracture reduction
- Recreate/accentuate the deformity and then correct
- For dorsally angulated fracture (Colles-type most common)
- Aggressive hyperextension/further dorsal displacement of the distal fragment
- Longitudinal traction
- Palmar translation of the distal fragment
- For volarly angulated fractures (less common)
- Aggressive flexion/further volar displacement of the distal fragment
- Longitudinal traction
- Dorsal translation of the distal fragment
-
Smith (DRF) Reduction Walkthrough
- Sugar tong splint
- Apply soft padding liberally over elbow, forearm, and palm up to the level of the distal palmar crease
- Measure plaster/Ortho-Glass from the mid-palm over the volar surface of the forearm, around the elbow, and over the dorsal surface of the forearm to the same level distally
- After wetting, lay the plaster/Ortho-Glass from the mid-palm over the volar surface of the forearm, around the elbow, and over the dorsal surface of the forearm to the same level distally.
- Make sure to keep plaster/Ortho-Glass off skin
- Wrap the splint with preferred elastic or non-elastic bandage.
- Mold the splint
- Reassess neurovascular status
Procedure Notes:
PROCEDURE NOTE Closed treatment of distal radial fracture (eg, Colles or Smith type) or epiphyseal separation, includes closed treatment of fracture of ulnar styloid, when performed; without manipulation.
PRE-PROCEDURE DIAGNOSIS: fracture of the *** distal radius
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of distal radial fracture (eg, Colles or Smith type) or epiphyseal separation, includes closed treatment of fracture of ulnar styloid, when performed; without manipulation.
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempt at reduction was made. A sugar tong splint was applied with a three-point mold. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** distal radius
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: None
NAME OF PROCEDURE: Closed treatment of distal radial fracture (eg, Colles or Smith type) or epiphyseal separation, includes closed treatment of fracture of ulnar styloid, when performed; without manipulation.
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to post-procedural pain, numbness, and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
No attempt at reduction was made. A sugar tong splint was applied with a three-point mold. Formal post reduction films showed unchanged alignment. The patient's neurovascular status was consistent with baseline.
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PROCEDURE NOTE - Closed treatment of distal radial fracture (eg, Colles or Smith type) or epiphyseal separation, includes closed treatment of fracture of ulnar styloid, when performed; with manipulation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** distal radius
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: Local anesthesia
NAME OF PROCEDURE: Closed treatment of distal radial fracture (eg, Colles or Smith type) or epiphyseal separation, includes closed treatment of fracture of ulnar styloid, when performed; with manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to median nerve compression or entrapment, post-procedural pain, and numbness and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
Using *** mL 1% lidocaine and *** mL of 0.25% marcaine, a hematoma block was performed under fluoroscopy. The *** distal radius was gently manipulated and fracture was reduced under fluoroscopy. A sugar tong splint was applied with a three-point mold. Fluoroscopic c-arm images were obtained as well as formal post reduction films which showed acceptable alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
PRE-PROCEDURE DIAGNOSIS: fracture of the *** distal radius
POST-PROCEDURE DIAGNOSIS: Same (refer above)
PROCEDURALIST: ***
ANESTHESIA: Local anesthesia
NAME OF PROCEDURE: Closed treatment of distal radial fracture (eg, Colles or Smith type) or epiphyseal separation, includes closed treatment of fracture of ulnar styloid, when performed; with manipulation
PROCEDURE IN DETAIL:
The risks and benefits of the procedure were discussed at length with the patient. Risks discussed included but were not limited to median nerve compression or entrapment, post-procedural pain, and numbness and stiffness. Following informed verbal consent after discussion of risks and benefits, the patient agreed to proceed with the procedure. A timeout was performed.
Using *** mL 1% lidocaine and *** mL of 0.25% marcaine, a hematoma block was performed under fluoroscopy. The *** distal radius was gently manipulated and fracture was reduced under fluoroscopy. A sugar tong splint was applied with a three-point mold. Fluoroscopic c-arm images were obtained as well as formal post reduction films which showed acceptable alignment. The patient's neurovascular status was consistent with baseline.
NUMBER OF REDUCTION ATTEMPTS: ***
COMPLICATIONS: ***
DISPOSITION:
Discharged home with follow up with orthopaedic surgery in 1 week for repeat evaluation
| Common ICD-10 Codes | Brief Description |
|---|---|
| S52.5 | Fracture of lower end of radius |
| S52.501 | Unspecified fracture of the lower end of right radius |
| S52.502 | Unspecified fracture of the lower end of left radius |
| S52.51 | fracture of the radial styloid process |
| S52.52 | Torus fracture of lower end of radius |
| S52.53 | Colles’ fracture |
| S52.54 | Smith’s fracture |
| S52.55 | Other extraarticular fracture of lower end of radius |
| S52.56 | Barton's fracture |
| S52.57 | Other intraarticular fracture of lower end of radius |
| S52.59 | Other fractures of lower end of radius |
- Principles of Casting and Splinting http://www.aafp.org/afp/2009/0101/p16.html Accessed April 4, 2020
- Hammert WC, Kramer RC, Graham B, Keith MW. AAOS appropriate use criteria: treatment of distal radius fractures. J Am Acad Orthop Surg. 2013;21(8):506-509. doi:10.5435/JAAOS-21-08-506
- Davenport M. Procedures for orthopedic emergencies. In: Bond M, ed. Orthopedic Emergencies: Expert Management for the Emergency Physician. Cambridge: Cambridge University Press; October 31, 2013.
- German C. Hand and wrist emergencies. In: Bond M, ed. Orthopedic Emergencies: Expert Management for the Emergency Physician. Cambridge: Cambridge University Press; October 31, 2013.


.webp)
.webp)